Everyone gets aches and pains over time, but if you experience pain across your whole body for a lengthy period, you may want to consult a medical practitioner. You may have a condition known as fibromyalgia. For people with fibromyalgia, the pain becomes a daily experience. According to U.S. National Institute of Arthritis and Musculoskeletal and Skin Diseases, women account for 80-90 percent of all fibromyalgia cases. Fibromyalgia greatly impacts on quality of patients’ life. What is Fibromyalgia Syndrome (FMS)? Fibromyalgia Syndrome (FMS) is a chronic condition causing pain, stiffness, and tenderness of the muscles, tendons, and joints. FMS triggers the central pain processing that produces heightened responses to painful sensor (hyperalgesia) and painful responses to non-painful sensor (allodynia) in our body. Other than lengthy pain all over body parts, people with FMS may also experience difficulty to sleep, fatigue, increased sensitivity to pain and muscle stiffness.
FMS is most common in women between the ages of 20 and 60, with most detected cases being at the age of 35. Only 1 out of 10 people with FMS are men. FMS rarely affects children.
What causes FMS? The cause of FMS is still not fully understood. Several factors such as dysfunction of the central and autonomic nervous systems, neurotransmitters, hormones, immune system, external stressors, psychiatric aspects, and others seem to be involved. After years of research by various organisations, a narrow list of factors is made. The US National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), and Arthritis Research UK suggest a few causal factors such as:
| Infections | Prior (any) infections may trigger FMS or make the symptoms worse |
| Genetics | If you have a family member with FMS, it is more likely for you to develop it |
| Trauma | Individuals who experience physical or emotional trauma may develop fibromyalgia. The condition has been linked with post-traumatic stress disorder |
| Stress | Stress has been linked to hormonal disturbances that contribute to FM |
So how can you know if you have FMS? Symptoms of FMS The symptoms tend to vary from person to person with the main symptoms outlined below:
| Widespread Pain | The pain is often described as a constant daily dull ache that has lasted for at least three months. To be considered widespread, the pain must occur on both sides of the body (symetrical) and, above and below the waist simultaneously. |
| Extreme Sensitivity | FMS can make you extremely sensitive to pain all over your body, and you may find that even the slightest touch is painful. If you hurt yourself, such as stubbing your toe, the pain may continue for much longer than it normally would. |
| Stiffness | FMS can make you feel stiff. The stiffness may be most severe when you’ve been in the same position for a long period of time – for example, when you first wake up in the morning. It can also cause your muscles to spasm, which is when they contract (squeeze) tightly and painfully. |
| Fatigue & Poor Sleep Quality | You often wake up tired, even though you have slept for a long period of time. Sleep is often disrupted by pain, and many patients with FMS have other sleep disorders, such as restless legs syndrome and sleep apnea. |
| Cognitive Complications | Typically known as “fibro fog”, you may find yourself having difficulty to focus, pay attention and concentrate on mental tasks. |
| IBS (Irritable Bowel Syndrome) | IBS is a common intestinal condition that causes abdominal pain and bloating. It commonly leads to constipation or diarrhea. |
| Other symptoms | Many people also experience depression, headaches, and menstrual pain or cramping in the lower abdomen |
There may be periods where the symptoms get better or worse, however, treatment is available to ease some of the symptoms, although the chances of it to disappear completely is unlikely. Diagnosis Previously, FMS is dismissed by doctors as a non-physical condition due to lack of medical evidence and any test to confirm the symptom of FMS, which for the most part is considered rather vague or too general. There is still lack of standardised set of diagnostic criteria. Nevertheless, medical colleges such as the American College of Rheumatology (ACR) produced some guides to help doctors. ACR’s Classification of Fibromyalgia includes the following criteria:
- – Widespread pain for at least three months, and
- – Pain is found in 11 out of 18 tender point sites on pressure, shown in the image below (called tender trigger points)
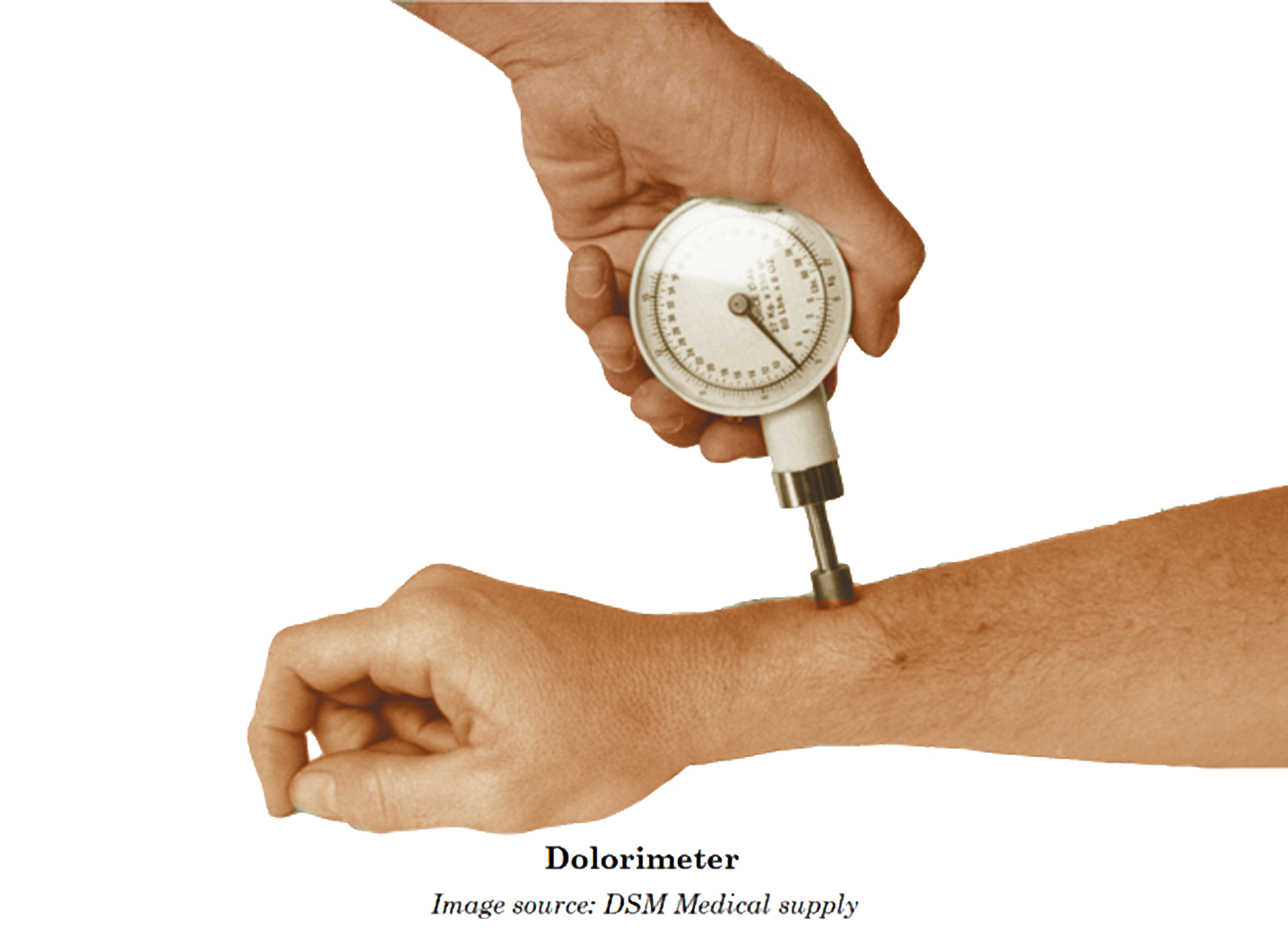
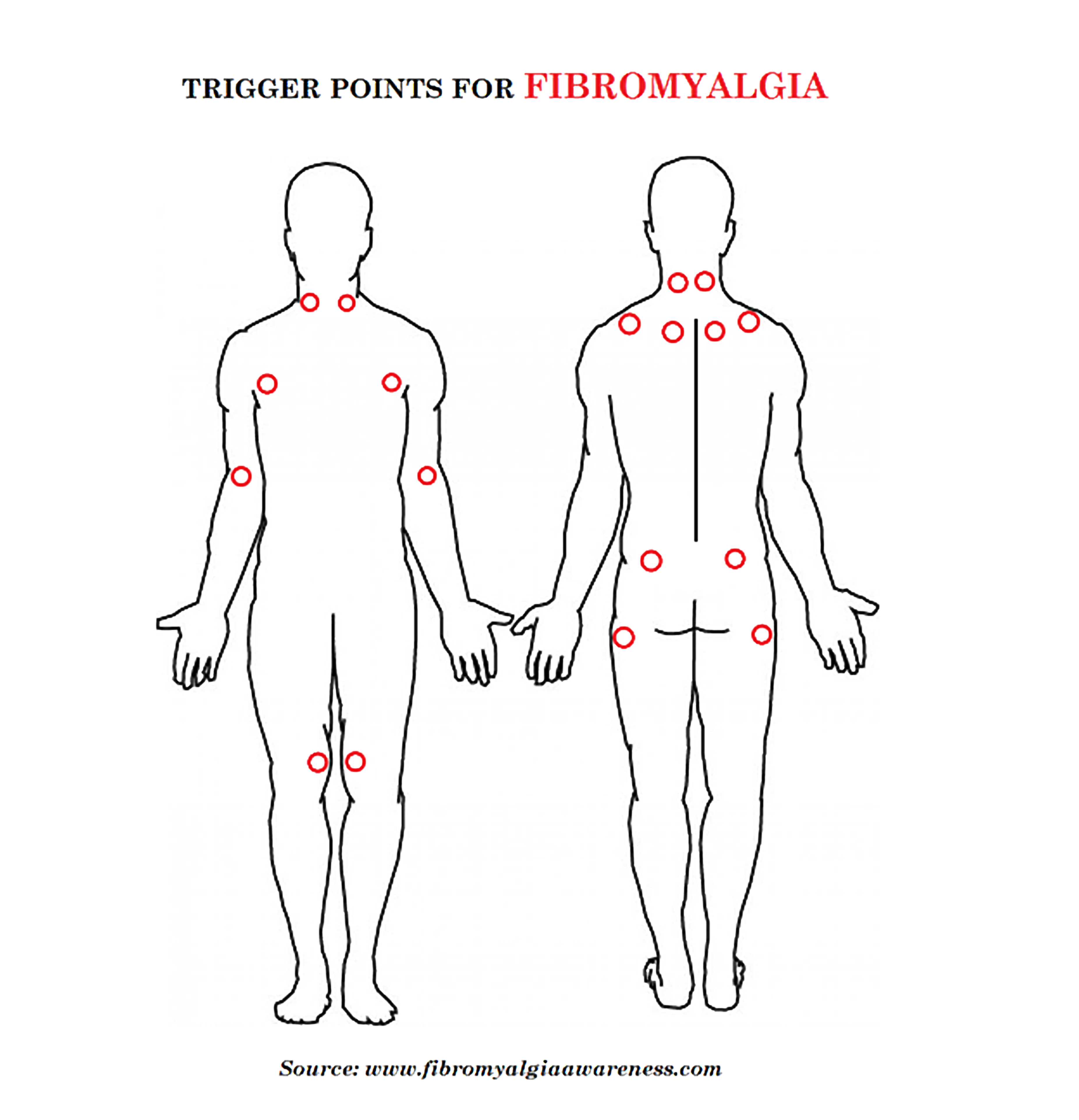 Through this assessment, pressure is applied onto the tender points with an instrument called Dolorimeter. The patients then need to state that the area is “painful” (“irritating” is not sufficient).
Through this assessment, pressure is applied onto the tender points with an instrument called Dolorimeter. The patients then need to state that the area is “painful” (“irritating” is not sufficient).
More recently, ACR has proposed that the tender point test to be replaced with a Widespread Pain Index (WPI) and Symptoms Severity (SS) scores. The one-page symptom checklist will hopefully be more suitable for use in the busy primary care setting. A focused physical exam and relevant investigations are still recommended to identify possible treatable causes for the patients’ symptoms. In place of the tender point count, patients (or their physician) may endorse 19 body regions in which pain has been experienced during the past one week. One point is given for each area, so the score is between 0-19. This number is referred to as the Widespread Pain Index (WPI). The SS score requires evaluation of four specific symptoms, on a scale of zero to three. These symptoms include:
- – Fatigue
- – Waking un-refreshed
- – Cognitive symptoms and
- – Somatic (physical) symptoms (such as headache, weakness, bowel problems, nausea, dizziness, numbness/tingling, hair loss).
The numbers assigned to each are added up, with total SS score from 0-12. The diagnosis, based on both the WPI score and the SS score, where high scores plus absent of treatable causes, confirm FMS. Treatment The goals of treatment in patients with FMS are to alleviate pain, increase restorative sleep, and improve physical function, ultimately optimising quality of life. Thus, your family doctor may coordinate the care with different disciplines of healthcare professionals. They are:
- – rheumatologist – doctor who manage diseases of muscles and joints
- – neurologist – doctor who take care of nervous system and pain
- – clinical psychologist – therapist on mental health problems
As FMS has numerous symptoms, no single treatment is effective for all. Treatments that work for some people may not necessarily work for others. A great majority of FMS patients can be managed well by family doctors at primary care clinics, by managing stress, depression, pain, supportive psychotherapy and life style modification. The cause of FMS is still not fully clear, but modern functional neuroimaging techniques are giving us important data about FMS. A multidisciplinary approach is optimal with the involvement of both drugs and non-drug treatment, such as aerobic exercise, strength training, aquatic exercises, cognitive-behavioral therapy, and also the emerging brain stimulation techniques. Most people with FMS find their symptoms get better over time through treatments and medications. But it is a long-term condition. The symptoms may come and go. The patient will probably have good days and bad days. Although FMS can be very miserable but it may help to know that it’s not a life-threatening disease. And it’s not a sign of damage to your joints or muscles.
Understanding your pain may help you worry about it less, and this may reduce the amount of pain you feel.
Bellato, E., Marini, E., Castoldi, F., Barbasetti, N., Mattei, L., Bonasia, D. E., & Blonna, D. (2012). Fibromyalgia Syndrome: Etiology, Pathogenesis, Diagnosis, and Treatment. Pain Research and Treatment. http://doi.org/10.1155/2012/426130 Hackshaw, Kevin V., Plans-Pujolras M., RodriguezSaona L. E., Moore M. A., Jackson E. K., Sforzo G. A., and Buffington T (2016). A pilot study of health and wellness coaching for fibromyalgia. BMC Musculoskeletal Disorders 17 (1): 457. http://www.everydayhealth.com/fibromyalgia/smiling-through-pain-living-on-air-with-fibromyalgia.aspx http://www.healthline.com/health/fibromyalgia http://www.mayoclinic.org/diseases-conditions/fibromyalgia/basics/tests-diagnosis/con-20019243 http://www.nhs.uk/Conditions/Fibromyalgia/Pages/Introduction.aspx Jahan, F., Nanji, K., Qidwai, W., & Qasim, R. (2012). Fibromyalgia Syndrome: An Overview of Pathophysiology, Diagnosis and Management. Oman Medical Journal, 27(3), 192–195. http://doi.org/10.5001/omj.2012.44 Prior Y. & Walker N. (2016). Rheumatology Occupational Therapy-led Fibromyalgia SelfManagement Education using Motivational Interviewing and Mindfulness Based Cognitive Therapy: A New Approach. Centre for Health Sciences Research Patient Information: Fibromyalgia (2016). BMJ Publishing Group Limited 2016. Related article: The Ultimate Guide to Travelling with Chronic Pain