Individuals with diabetes face a host of problems from their inability to process excess sugar in their bloodstream. Not only does it disrupt the vascular system, it affects the eyes, kidneys, legs and feet. Diabetes can also lead to slower healing time, thereby increasing the risk of infection. It is no surprise that foot ulceration, sepsis, and subsequent amputation are known and feared by almost every person diagnosed with diabetes. Yet these are preventable with adequate education and timely care. This is where the podiatrist is your best port of specialist care.
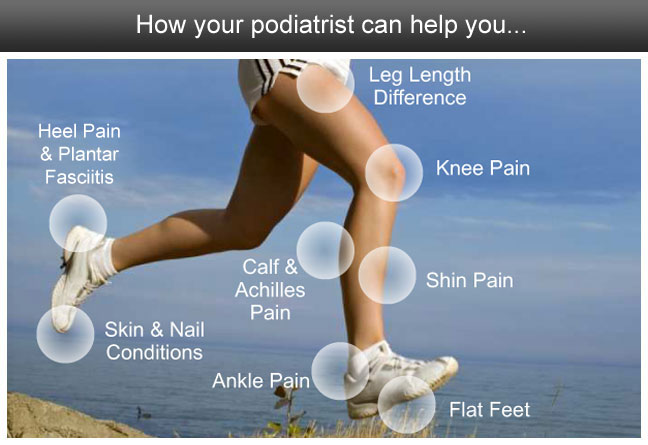
A podiatrist will assess your feet to diagnose and treat foot and lower limb problems. These may include skin and nail problems, foot and ankle injuries, foot complications related to diabetes as well as problems with biomechanics. They will also manage diabetic ulcers to prevent limb amputation.
Podiatrists, in essence, play a crucial role in monitoring and managing lower limb issues to ensure an individual is able to continue to be active on his/her feet. Therefore, patient demographics can be diverse; ranging from monitoring children’s growth and development, managing sports injuries, working with people with chronic disease, disability and the ageing population. Podiatrists are experts in wound and pain management of the lower limbs.
Diabetes Foot Care People often perceive feet and lower limb ailments as less critical, compared to the heart, face or eyes. Additionally, many are still unaware that podiatrists provide vital support for diabetic individuals who reflect a higher incidence of all reported lower limb and feet related problems, including serious ulcerations and amputation. So diabetic foot ulcers are often brought to the podiatrist attention rather late in the game, resulting in more complicated and prolonged treatment regime. A simple example would be an individual with diabetes who works in construction or a hawker who is on his/her feet throughout the day. The job nature puts them at higher risk of sharp or heavy objects dropping on the foot or hot water scalding injuries. For these individuals, podiatrists would recommend protective shoes and insoles as well as seamless socks, a mainstay of preventing foot injuries.
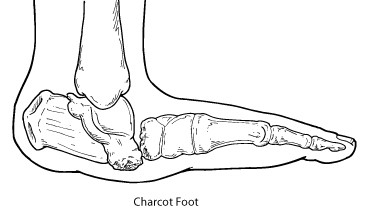
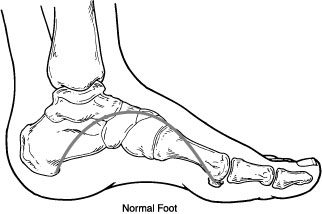
Another diabetic complication is charcot foot which is a serious condition that can lead to severe foot deformity. Charcot foot is a condition causing inflammation of the foot that can occur in people who have significant nerve damage (neuropathy). This decrease in sensation and the ability to feel temperature, pain, or trauma may result in the patient continuing to walk—making the injury worse. It is thus extremely important that patients with diabetes – a disease often associated with neuropathy – take preventive measures and seek immediate care if any abnormalities appear. Early signs of Charcot foot may include redness, swelling, and increased temperature of the foot. If diagnosed early, the most important immediate treatment for the active Charcot foot is offloading.
 |
 |
Poor blood circulation means not enough blood flows to your external limbs, making it hard for a sore to heal. This problem is called peripheral artery disease (PAD). So for diabetics, it is recommended that even for common foot problems, such as corn and callus, blisters, ingrown toenails, bunions, warts, and fungal infection it is best to resist that temptation to go to the nearest pharmacy and get an off-the-counter solution. It is best to get prompt treatment from a podiatrist.
Diabetic moms who love going for pedicures or foot spas are advised to be extremely careful as to how their feet are managed to prevent problems such as fungal or ingrown nails, or even unwanted nicks or abrasions. In incidences where vascular disease is present, it may delay healing of wounds. Prolonged non-healing ulceration increases infection risk and complicates the treatment plan.
Podiatrists are experts in biomechanics, observing how an individual walks. They may recommend special shoes, prescribe orthotic devices or even a pressure sock. They work at educating the person and their caregivers about following appropriate guidelines to reduce the foot pain or pressure on the wound. For the diabetics who are also sport enthusiasts, seeing a podiatrist regularly can help with preventing and treating injuries related to sports and/or exercise. A podiatrist would be able to share how preventive care can help improve efficiency and foot function. Podiatrists also assesses the individual’s post-wound rehabilitation. Routine podiatric treatment prevents re-ulceration and improves foot function by special orthotics, shoe modifications and lifestyle management.
So even if you think your feet are in good shape, you should consider visiting your podiatrist for an assessment and to have the hard skin on your feet removed, toenails clipped or just to find out if you’re wearing the right shoes (take your shoes with you – especially moms who love high heels – for specific advice on footwear). Your podiatrist will be more than willing to craft a management plan just for you. After all as the Roman lyric poet, Horace, once said: A shoe that is too large is apt to trip one, and when too small, to pinch the feet. So it is with those whose fortune does not suit them.
This article is brought to you by IMU Healthcare.