25 – 27 September 2014 – As part of the 15th IMU MBBS Anniversary, the International Medical University organised a National Clinical Skills Conference held at Royale Bintang Hotel and at its Clinical School in Seremban. The pre-conference was on 25 September 2014 and this started with 4 concurrent and well – attended workshops held at IMU Clinical School campus.
25 – 27 September 2014 – As part of the 15th IMU MBBS Anniversary, the International Medical University organised a National Clinical Skills Conference held at Royale Bintang Hotel and at its Clinical School in Seremban. The pre-conference was on 25 September 2014 and this started with 4 concurrent and well – attended workshops held at IMU Clinical School campus.
The following day was the conference at Royale Bintang Hotel. YBhg Dato’ Dr Zailan bt Dato’ Hj Adnan, State Health Director of Negeri Sembilan Health Department officiated the event. Guest speakers from Ministry of Health, Institut Jantung Negara (IJN) and Director of ACT Mental Health in Australia, Dr Peter Norrie, imparted their knowledge and experience to the audience.
After the morning lectures, participants were then broken into groups of 10 and moved from station to station to have hands-on experience in various areas of clinical skills.
On the night of the first day, all participants and IMU staff were at the 15th IMU MBBS Anniversary Dinner at the same hotel. The grand affair was officiated by a representative of the Menteri Besar, Negeri Sembilan, YB Dato’ Dr Hj Awaludin Bin Said who is the Yang Dipertua Dewan Undangan Negeri. The audience were entertained by the talented IMU students who really mesmerized the crowd with their performances.
On the following day, after the didactic lectures in the morning, the last and final part of the hands-on activities were conducted at the IMU Clinical School in Seremban. Feedback from the delegates on this conference were largely positive and congratulatory. 
 Proceedings of the Conference are summarised by student volunteers and are as stated below: Pre-conference – 25 September 2014 TITLE: Managing Opioid Dependence in Primary Care – NDST FACILITATOR: A/Prof Philip George
Proceedings of the Conference are summarised by student volunteers and are as stated below: Pre-conference – 25 September 2014 TITLE: Managing Opioid Dependence in Primary Care – NDST FACILITATOR: A/Prof Philip George  The speaker first discussed about the pathophysiology of opioid dependence. The reward pathway and how opioid affects it was discussed in depth. The issue of opioid management was discussed in accordance to the biopsychosocial model. The biological part of managing a patient who is opioid dependent, treatment using methadone was explored. The speaker also spoke about the use of methadone in pregnancy and mothers who are currently breast-feeding. As for the psychosocial management, the cognitive behavior therapy was discussed. At the end of the session, a forum was held. Participants shared their experience in running the methadone clinic. They were also given the opportunity to ask questions. In conclusion, the talk was very beneficial and the participants enjoyed and learnt a lot from the talk. TITLE: Management of Medical Emergencies FACILITATORS: Dr Thiruselvi Subramaniam and Dr Tan Ann Jee
The speaker first discussed about the pathophysiology of opioid dependence. The reward pathway and how opioid affects it was discussed in depth. The issue of opioid management was discussed in accordance to the biopsychosocial model. The biological part of managing a patient who is opioid dependent, treatment using methadone was explored. The speaker also spoke about the use of methadone in pregnancy and mothers who are currently breast-feeding. As for the psychosocial management, the cognitive behavior therapy was discussed. At the end of the session, a forum was held. Participants shared their experience in running the methadone clinic. They were also given the opportunity to ask questions. In conclusion, the talk was very beneficial and the participants enjoyed and learnt a lot from the talk. TITLE: Management of Medical Emergencies FACILITATORS: Dr Thiruselvi Subramaniam and Dr Tan Ann Jee  Medical emergencies are part and parcel of everyday hospital life and a good knowledge of adult life support is vital to bring the patient out of the danger zone. This half-a-day course aims to recap and reinforce the knowledge and skills that the participants had in managing emergencies. During the briefing, the participants were faced with two obstetrical emergencies. It was unexpected and everyone were fumbling, trying their best to salvage the patient’s life. After the frenzy, Dr Thiruselvi Subramaniam and Dr Tan Ann Jee brought the participants through a refresher course in airway management and cardiac life support. The participants were enthusiastic and made full use of the time in brushing up the skills. They were then required to manage two different emergencies – asthma and motor vehicle accident in the simulation ward and the simulation operation theatre respectively. Although challenging, the participants managed to fulfill the required tasks on the sophisticated manikins. It was a thrilling and rewarding experience for participants. Feedback from these participants were that they would like to attend similar one-day workshops in the future. The hard work of facilitators and student helpers and the enthusiasm of the participants certainly made the workshop a success. As reported by Lim Sean Yee and Syahidah bt Mohd Noh TITLE: Clinical Approach to Chest and Abdominal Radiograph FACILITATORS: A/Prof Rohaizan Yunus and Dr Nalini Somawera
Medical emergencies are part and parcel of everyday hospital life and a good knowledge of adult life support is vital to bring the patient out of the danger zone. This half-a-day course aims to recap and reinforce the knowledge and skills that the participants had in managing emergencies. During the briefing, the participants were faced with two obstetrical emergencies. It was unexpected and everyone were fumbling, trying their best to salvage the patient’s life. After the frenzy, Dr Thiruselvi Subramaniam and Dr Tan Ann Jee brought the participants through a refresher course in airway management and cardiac life support. The participants were enthusiastic and made full use of the time in brushing up the skills. They were then required to manage two different emergencies – asthma and motor vehicle accident in the simulation ward and the simulation operation theatre respectively. Although challenging, the participants managed to fulfill the required tasks on the sophisticated manikins. It was a thrilling and rewarding experience for participants. Feedback from these participants were that they would like to attend similar one-day workshops in the future. The hard work of facilitators and student helpers and the enthusiasm of the participants certainly made the workshop a success. As reported by Lim Sean Yee and Syahidah bt Mohd Noh TITLE: Clinical Approach to Chest and Abdominal Radiograph FACILITATORS: A/Prof Rohaizan Yunus and Dr Nalini Somawera 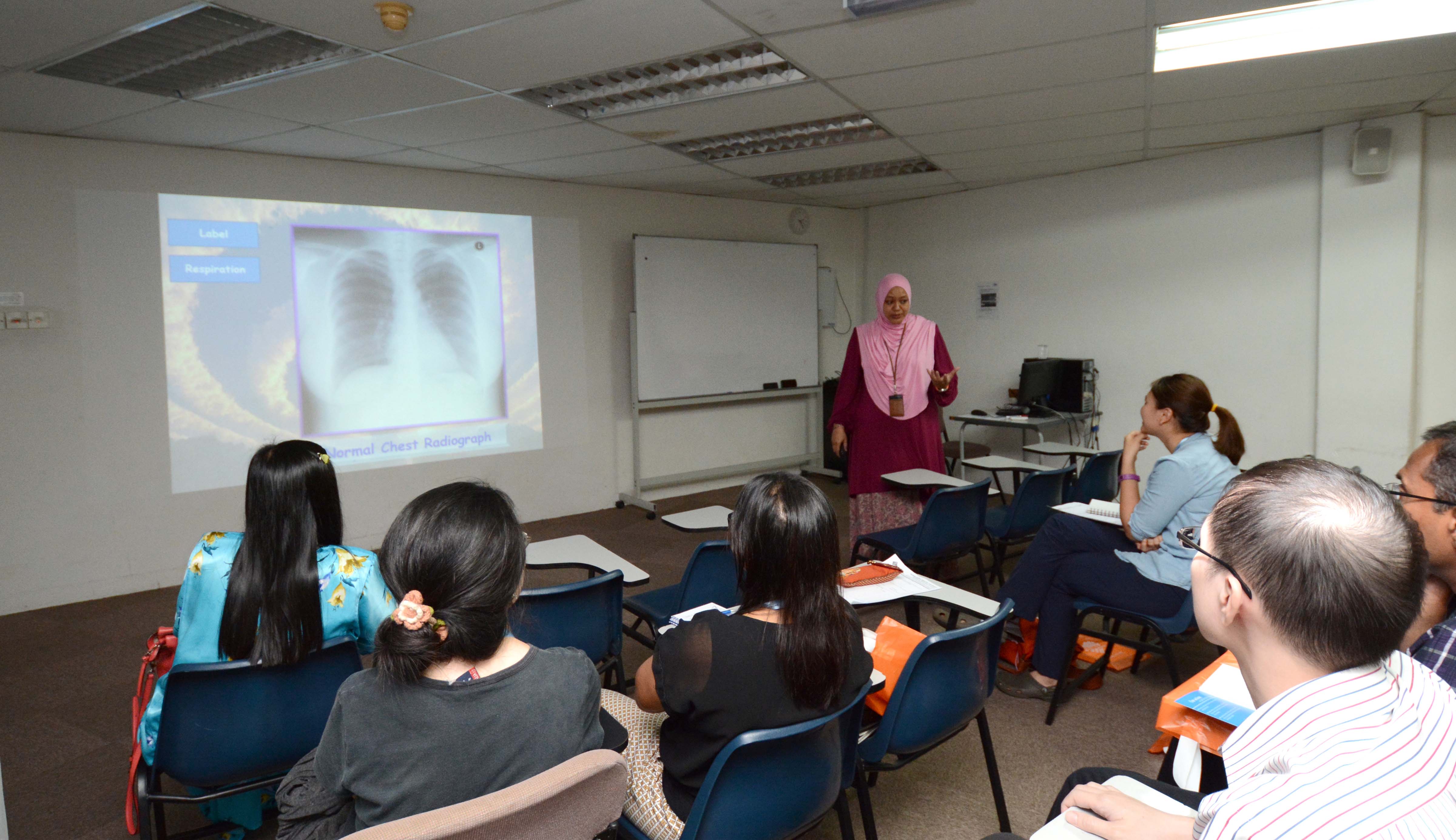 This session was divided into two parts: theory and practical. The first part started with participants being taught the approach and were guided on how to interpret chest and abdominal radiographs. Participants were reminded of the need of a systematic approach when interpreting radiographs. For the next half of the session, participants were shown various radiographs and asked to interpret their findings. Throughout the session, the importance of a good history and clinical examination were emphasised. With both of these, a clinical diagnosis could be made and relevant imaging studies can carried out. Participants were encouraged to apply their basic sciences and reflect on the pathophysiology of the disease to guide them on the expected findings. This is vital in order not to miss out important findings on the radiograph(s). It was also emphasised that radiographs are to support the diagnosis made. The next session saw participants gathering in groups to discuss the findings and diagnosis of various cases. This provided a platform for exchange of ideas and gave participants the opportunity to learn from others with different clinical experience and background. Overall, participants were enriched by the session and motivated to approach and interpret chest and abdominal radiographs in a different light. As reported by Eunice Ann Loh TITLE: Fetal Morphology FACILITATOR: A/Prof Nazimah Idris
This session was divided into two parts: theory and practical. The first part started with participants being taught the approach and were guided on how to interpret chest and abdominal radiographs. Participants were reminded of the need of a systematic approach when interpreting radiographs. For the next half of the session, participants were shown various radiographs and asked to interpret their findings. Throughout the session, the importance of a good history and clinical examination were emphasised. With both of these, a clinical diagnosis could be made and relevant imaging studies can carried out. Participants were encouraged to apply their basic sciences and reflect on the pathophysiology of the disease to guide them on the expected findings. This is vital in order not to miss out important findings on the radiograph(s). It was also emphasised that radiographs are to support the diagnosis made. The next session saw participants gathering in groups to discuss the findings and diagnosis of various cases. This provided a platform for exchange of ideas and gave participants the opportunity to learn from others with different clinical experience and background. Overall, participants were enriched by the session and motivated to approach and interpret chest and abdominal radiographs in a different light. As reported by Eunice Ann Loh TITLE: Fetal Morphology FACILITATOR: A/Prof Nazimah Idris  A/Prof Nazimah started the session with a brief introduction about the importance of using ultrasound to assess fetal developmental status and assure mothers on the wellbeing of their babies. Throughout the session, a book on fetal morphology was passed among the participants to get a clue of fetal morphology. Prof Nazimah later explained proper sequence of doing ultrasound and what organ they should expect to see. The head circumference, genital organ, and even the genetic deformity picture of fetal were demonstrated clearly to participants. A/Prof Nazimah also told us the importance of doing a detailed scan for the pregnant mother and to intervene early if they found abnormality in the developmental of the fetal. After a brief introduction about the picture of fetal morphology, participants were divided into four groups; each group consists of three doctors to ensure quality of training. The four stations were each manned by A/Prof Nazimah, Dr Kavitha, Dr Krishna and Dr Bheena respectively. They showed the participants the correct technique of performing a fetal morphology ultrasound scan and pointed out important and easily missed mistakes. Participants were allowed to perform ultrasound scan on their own under the guidance of A/Prof Nazimah. The facilitators provided guidance on the way to hold the probe, head circumference measurement, fetal heart sounds, resistance index and many more. The hands-on session allowed participants to apply what they have learned. As reported by Chua Chen Zhi Main Conference Day 1 – 26 September 2014 TITLE: The Difficult Patient SPEAKER: Prof Kwa Siew Kim
A/Prof Nazimah started the session with a brief introduction about the importance of using ultrasound to assess fetal developmental status and assure mothers on the wellbeing of their babies. Throughout the session, a book on fetal morphology was passed among the participants to get a clue of fetal morphology. Prof Nazimah later explained proper sequence of doing ultrasound and what organ they should expect to see. The head circumference, genital organ, and even the genetic deformity picture of fetal were demonstrated clearly to participants. A/Prof Nazimah also told us the importance of doing a detailed scan for the pregnant mother and to intervene early if they found abnormality in the developmental of the fetal. After a brief introduction about the picture of fetal morphology, participants were divided into four groups; each group consists of three doctors to ensure quality of training. The four stations were each manned by A/Prof Nazimah, Dr Kavitha, Dr Krishna and Dr Bheena respectively. They showed the participants the correct technique of performing a fetal morphology ultrasound scan and pointed out important and easily missed mistakes. Participants were allowed to perform ultrasound scan on their own under the guidance of A/Prof Nazimah. The facilitators provided guidance on the way to hold the probe, head circumference measurement, fetal heart sounds, resistance index and many more. The hands-on session allowed participants to apply what they have learned. As reported by Chua Chen Zhi Main Conference Day 1 – 26 September 2014 TITLE: The Difficult Patient SPEAKER: Prof Kwa Siew Kim  The speaker started off with the definition of difficult patients and the labels that are put on them. Difficult patients are medically challenging patients who usually come with multiple problems, lack social support, have interpersonal problems and may be psychiatrically ill. We sometimes refer to these patients with social and communication problems as “heartsink” patients. However, the problems do not lie exclusively with patients. “What type of doctor has more difficult patients?” The speaker stated that healthcare givers with high workload and poor social skills usually encounter a greater number of difficult patients. Institutional factors such as long waiting time, shortage of doctors or beds and rationing of medications and services can also give rise to agitated and angry patients. To deal with them, we have to improve our communication skills and take into consideration the special circumstances of the patient and his environment. We need to acknowledge patient’s feelings and address their issues. We should also not forget to explore patient’s ideas, concern and expectation (ICE). Before the speaker ended her speech, she advised doctors to seek help from their peers or superior if they encounter challenging and problematic patients whom they cannot handle. They could refer such patients to their more experienced colleagues and to attend communication skill courses. As reported by Soh Wan Wen TITLE: Recovery in Mental Health – The Australian Experience SPEAKER: Dr Peter Norrie
The speaker started off with the definition of difficult patients and the labels that are put on them. Difficult patients are medically challenging patients who usually come with multiple problems, lack social support, have interpersonal problems and may be psychiatrically ill. We sometimes refer to these patients with social and communication problems as “heartsink” patients. However, the problems do not lie exclusively with patients. “What type of doctor has more difficult patients?” The speaker stated that healthcare givers with high workload and poor social skills usually encounter a greater number of difficult patients. Institutional factors such as long waiting time, shortage of doctors or beds and rationing of medications and services can also give rise to agitated and angry patients. To deal with them, we have to improve our communication skills and take into consideration the special circumstances of the patient and his environment. We need to acknowledge patient’s feelings and address their issues. We should also not forget to explore patient’s ideas, concern and expectation (ICE). Before the speaker ended her speech, she advised doctors to seek help from their peers or superior if they encounter challenging and problematic patients whom they cannot handle. They could refer such patients to their more experienced colleagues and to attend communication skill courses. As reported by Soh Wan Wen TITLE: Recovery in Mental Health – The Australian Experience SPEAKER: Dr Peter Norrie  Mental health has always been a topic of taboo in Malaysia. There are various approaches taken by medical practitioners and other organisations to improve the care and services provided to individuals who require intervention. The structure of the talk was as such where recovery was introduced from all aspects possible ie community integration, medications and a multi-focused approach inclusive of professionals, consumers and carers. The importance of inter-professional work was emphasised as it has produced the best outcome. Moreover, this approach enables patient’s individual personalities to be taken into consideration when the plan of care is structured for the patient’s recovery. The recovery of patients is usually assessed on a sliding scale as even a relative recovery would indicate a better quality of life for the respective individual. Dr Peter showed the audience a comprehensive guide to recovery in terms of mental health and was able to encourage the consideration of all aspects in the treatment of a patient with mental health disabilities. As reported by Reena Priya TITLE: Systemic Clinical Approach of Paediatric Chest and Abdominal Radiograph SPEAKER: A/Prof Rohaizan Yunus The participants were first introduced to the important concept that children are not small adults. The unique anatomical and physiological features of children require special consideration in the clinical approach in chest and abdominal radiograph. Besides this, the correlation between the clinical presentation and radiological features is very important for the diagnosis and the management.
Mental health has always been a topic of taboo in Malaysia. There are various approaches taken by medical practitioners and other organisations to improve the care and services provided to individuals who require intervention. The structure of the talk was as such where recovery was introduced from all aspects possible ie community integration, medications and a multi-focused approach inclusive of professionals, consumers and carers. The importance of inter-professional work was emphasised as it has produced the best outcome. Moreover, this approach enables patient’s individual personalities to be taken into consideration when the plan of care is structured for the patient’s recovery. The recovery of patients is usually assessed on a sliding scale as even a relative recovery would indicate a better quality of life for the respective individual. Dr Peter showed the audience a comprehensive guide to recovery in terms of mental health and was able to encourage the consideration of all aspects in the treatment of a patient with mental health disabilities. As reported by Reena Priya TITLE: Systemic Clinical Approach of Paediatric Chest and Abdominal Radiograph SPEAKER: A/Prof Rohaizan Yunus The participants were first introduced to the important concept that children are not small adults. The unique anatomical and physiological features of children require special consideration in the clinical approach in chest and abdominal radiograph. Besides this, the correlation between the clinical presentation and radiological features is very important for the diagnosis and the management.  After we have made the clinical diagnosis, we should focus on signs on the radiograph which can confirm the final diagnosis by taking pathophysiological process into consideration. The understanding of embryological development and anatomical landmarks are also essential in the interpretation of the radiograph. Anteroposterior view (supine) is the main view in chest radiograph among pediatric age group because they are not able to stand. Similarly, the projection mainly used in abdominal radiograph is anteroposterior (supine) view because supine radiograph provides more information compared with erect position. However, be aware that babies may move when radiographs are being taken and this may interfere with the radiological interpretation. For the interpretation of the abdominal radiograph, we should see the distribution and the content of the bowel loops, the dilatation and separation of the bowel loops, the intraluminal and extra-luminal bowel gas and soft tissues.
After we have made the clinical diagnosis, we should focus on signs on the radiograph which can confirm the final diagnosis by taking pathophysiological process into consideration. The understanding of embryological development and anatomical landmarks are also essential in the interpretation of the radiograph. Anteroposterior view (supine) is the main view in chest radiograph among pediatric age group because they are not able to stand. Similarly, the projection mainly used in abdominal radiograph is anteroposterior (supine) view because supine radiograph provides more information compared with erect position. However, be aware that babies may move when radiographs are being taken and this may interfere with the radiological interpretation. For the interpretation of the abdominal radiograph, we should see the distribution and the content of the bowel loops, the dilatation and separation of the bowel loops, the intraluminal and extra-luminal bowel gas and soft tissues.
In conclusion, we interpret a radiograph by correlating the clinical manifestation of patient with the signs seen on the radiograph.
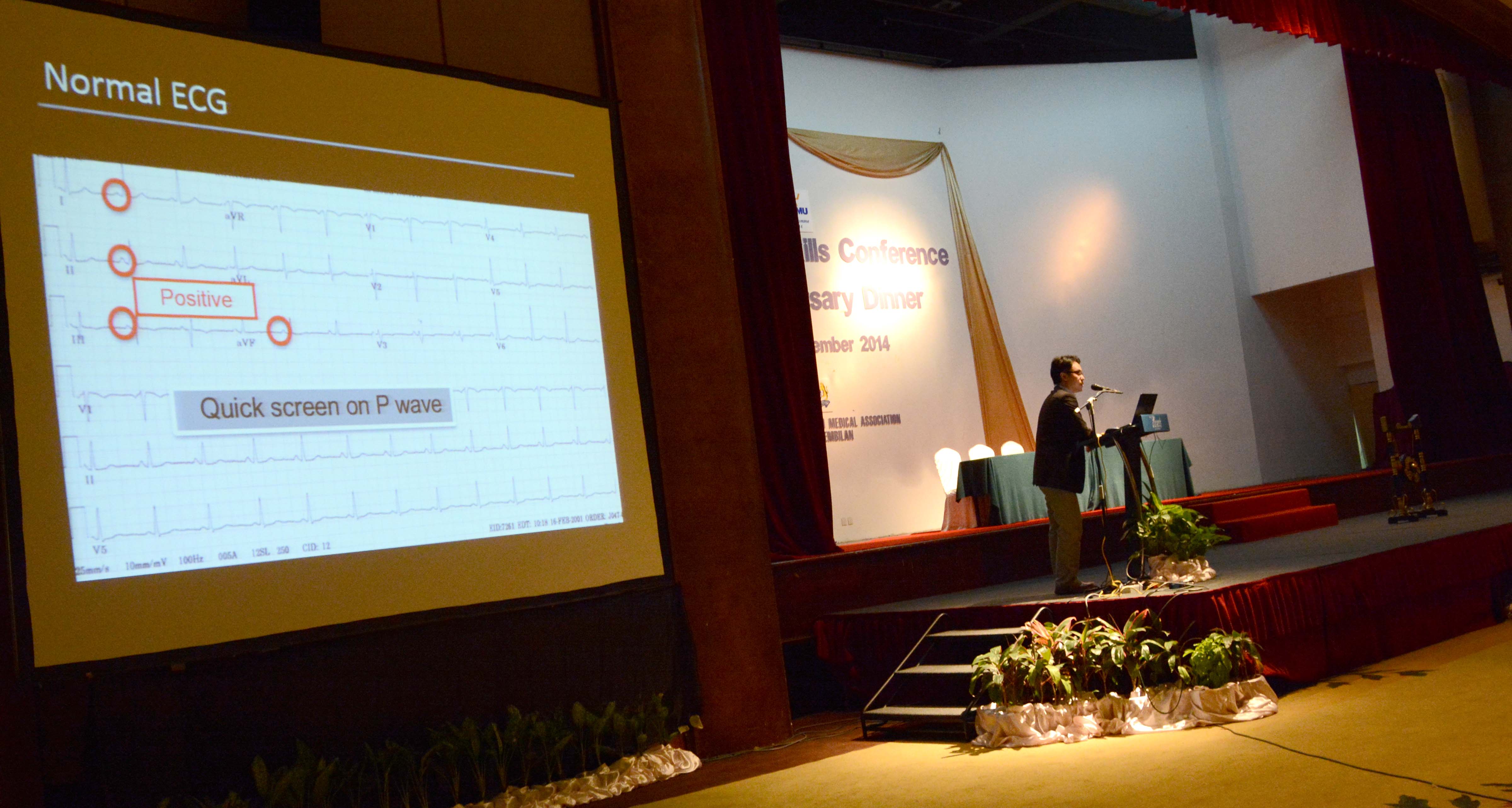
As reported by Lim Fang Chan TITLE: Electrocardiographic Evaluation of Tachyarrhythmia SPEAKER: Dr Koh Kok Wei In this symposium, the speaker recapitulated the normal ECG pattern, specifically the axis, P wave, QRS complex and P-R interval. He categorised tachyarrhythmia into supraventricular origin and ventricular origin. Supraventricular tachyarrhythmia is abnormal rhythm from sinus node, atrium and AV node, while fascicles, bundle branches Purkinje fibers and ventricles cause ventricular tachyarrhythmia. Tachycardia can also be classified into narrow or wide QRS tachycardia.
“How to identify a ventricular tachycardia (VT)?” Firstly, identify patients with high risk factors which includes patients with structural heart disease, hemodynamic unstable, history of syncope family history of sudden cardiac death or genetic heart disease and patients who are on antiarrhythmics. The ECG changes that are suggestive of VT are AV dissociation, positive QRS axis in AVR lead, presence of capture beat or fusion beat and precordial concordance. To evaluate tachyarrhythmia, we need to ensure the patient’s stability, identify his comorbidity and read his ECG sensibly. Finally, the speaker emphasised that in any circumstances, we always have to treat the patient as a whole, not the ECG.
As reported by Soh Wan Wen TITLE: Small Hole Big Problem SPEAKER: Dr Valuyeetham K Ambu Ear discharge or otorrhoea is a very common symptom in clinical practice. It should not be only treated symptomatically by giving antibiotics to the patient but to treat the underlying problem of the infection. The symptom must be taken seriously before the hearing loss becomes irreversible. We must first know what we want to look for anatomically before examining the eardrum to find the pathology. The important bony landmark (white dot), is the lateral process of the malleus which is never lost no matter how bad the infection is. If a line is drawn across the white dot, the part below will be the pars densa (three layers and very strong), which is usually seen through otoscope. It is important not to forget the part above the white dot, pars flaccida (two layers, soft) which is easily retracted. If the infection occurs in pars flaccid; the purulent, pus-like discharge can never come from middle ear, it is usually caused by staphylococcus infection or furuncles in the skin (squamous cell epithelium) of external ear canal. However, whenever there is mucus-like, mucoid or muco-purulent discharge, it usually comes from middle ear. Scanty and foul-smelling ear discharge classically indicates cholesteatoma.  Another cause of scanty ear discharge will be blood stain in the ear (osteomyelitis or malignancy). If there is swollen, red and inflamed external ear canal, this will be typical otitis externa. If you see a small bump in the posterior wall with hairs surrounding it, this will be localised otitis externa which is most commonly furuncle (infection of the hair follicles). There are two types of diseases in middle ear; one is tympanic membrane disease, which is usually caused by Eustachian tube pathology (negative pressure). Most of the perforation is central (there will be ring of tympanic membrane all around the perforation). If the perforation is marginal involving the bone, bone is exposed to the infection and eventually results in osteomyelitis and bone erosion. Otitis media is clearly seen as inflamed red intact eardrum. 80% of acute otitis media is caused by virus, thus it isuseless to prescribe antibiotics and they are self-limiting. Thin, dry, perforated eardrum should be closed by operation, because hearing aids are somehow needed. A poor eardrum will require an increased amplification and increased amplification will cause distorted sound. Good eardrum works better for hearing aids. Sometimes, a huge perforation will expose the middle ear structures such as stapes and round window. The perforation is still considered safe when there is still tympanic membrane lining protecting the bone from infection. Remember to give antibiotics and keep the ear drum dry. If the infection affects the bone; bone conduction is affected and this results in sensorineural hearing loss. Cholesteatoma is a destructive and expanding growth consisting of keratinizing squamous epithelium in the middle ear and/or mastoid process. Although these are not strictly speaking tumours or cancers they can still cause significant problems because of their erosive and expansile properties resulting in the destruction of the ossicles as well as their possible spread through the base of the skull into the brain. They are also often infected and result in chronically draining ears. Earwax should be removed on the attic to see whether there is a small hole underneath the earwax which erodes the bony structure. In conclusion, a small hole above the white dot is considered unsafe and this may be a big problem with severe complications such as bone erosion. As reported by Lim Fang Chan Clinical Skills – Hands-on TITLE: Medical Certificate Seeker FACILITATOR: A/Prof Anthony
Another cause of scanty ear discharge will be blood stain in the ear (osteomyelitis or malignancy). If there is swollen, red and inflamed external ear canal, this will be typical otitis externa. If you see a small bump in the posterior wall with hairs surrounding it, this will be localised otitis externa which is most commonly furuncle (infection of the hair follicles). There are two types of diseases in middle ear; one is tympanic membrane disease, which is usually caused by Eustachian tube pathology (negative pressure). Most of the perforation is central (there will be ring of tympanic membrane all around the perforation). If the perforation is marginal involving the bone, bone is exposed to the infection and eventually results in osteomyelitis and bone erosion. Otitis media is clearly seen as inflamed red intact eardrum. 80% of acute otitis media is caused by virus, thus it isuseless to prescribe antibiotics and they are self-limiting. Thin, dry, perforated eardrum should be closed by operation, because hearing aids are somehow needed. A poor eardrum will require an increased amplification and increased amplification will cause distorted sound. Good eardrum works better for hearing aids. Sometimes, a huge perforation will expose the middle ear structures such as stapes and round window. The perforation is still considered safe when there is still tympanic membrane lining protecting the bone from infection. Remember to give antibiotics and keep the ear drum dry. If the infection affects the bone; bone conduction is affected and this results in sensorineural hearing loss. Cholesteatoma is a destructive and expanding growth consisting of keratinizing squamous epithelium in the middle ear and/or mastoid process. Although these are not strictly speaking tumours or cancers they can still cause significant problems because of their erosive and expansile properties resulting in the destruction of the ossicles as well as their possible spread through the base of the skull into the brain. They are also often infected and result in chronically draining ears. Earwax should be removed on the attic to see whether there is a small hole underneath the earwax which erodes the bony structure. In conclusion, a small hole above the white dot is considered unsafe and this may be a big problem with severe complications such as bone erosion. As reported by Lim Fang Chan Clinical Skills – Hands-on TITLE: Medical Certificate Seeker FACILITATOR: A/Prof Anthony  The aim of this station was to create awareness that repeated seekers of medical certificate should not be taken lightly. It was a forty minutes role-playing station. The participants were allowed to interview a simulated patient (who was a repeated medical certificate seeker) for the first 16 minutes. The speaker observed their interviewing techniques as well as their ability to manage a patient who repeatedly sought medical leave as he had an underlying psychosocial problem (he is a gay who has been exposed at work through his Facebook account). After that the speaker suggested areas for improvement as well as discussed the importance of identifying an individual with an underlying problem at a primary care level. The take home message from the session was to look for an underlying cause and to develop communication skills with a patient who repeatedly asks for medical leave. TITLE: Interpreting Paediatric Chest and Abdominal Radiograph FACILITATOR: A/Prof Rohaizan Yunus Paediatric age group spans from newborn up to the mature age of 18 and they present with diseases that were different from the adult population. A good knowledge of interpreting paediatric radiological images is vital in successful management of their conditions. As the participants had attended the talk on this topic in the morning, they are now required to interpret the chest and abdominal radiographs given and draw on the diagnoses.
The aim of this station was to create awareness that repeated seekers of medical certificate should not be taken lightly. It was a forty minutes role-playing station. The participants were allowed to interview a simulated patient (who was a repeated medical certificate seeker) for the first 16 minutes. The speaker observed their interviewing techniques as well as their ability to manage a patient who repeatedly sought medical leave as he had an underlying psychosocial problem (he is a gay who has been exposed at work through his Facebook account). After that the speaker suggested areas for improvement as well as discussed the importance of identifying an individual with an underlying problem at a primary care level. The take home message from the session was to look for an underlying cause and to develop communication skills with a patient who repeatedly asks for medical leave. TITLE: Interpreting Paediatric Chest and Abdominal Radiograph FACILITATOR: A/Prof Rohaizan Yunus Paediatric age group spans from newborn up to the mature age of 18 and they present with diseases that were different from the adult population. A good knowledge of interpreting paediatric radiological images is vital in successful management of their conditions. As the participants had attended the talk on this topic in the morning, they are now required to interpret the chest and abdominal radiographs given and draw on the diagnoses.  Each participant has his own way to approach these black and white films but A/Prof Rohaizan offered to guide them with a different approach – “Formulate your differential diagnoses from the summary given, and use the radiographs as a tool to refine it”. It was no easy task to adopt a new approach and the discussion was paused by a few awkward silences. However, the participants started to express their excitement as they began to appreciate the radiographs in a new light – early bronchopneumonic changes secondary to viral upper respiratory tract infection, appendicitis secondary to appendicolith causing pericolic abscess and small bowel obstruction, just to name a few. At the end of the station, the participants were exposed to radiographs of bronchopneumonia, acute laryngotracheobronchitis, acute epiglottitis, appendicitis, and intussusception. They could not hide their satisfactions after the fruitful discussion and wished to have more time to discuss more scenarios. As reported by Lim Sean Yee and Syahidah bt Mohd Noh TITLE: Assessing Depression and Suicide in Primary Care FACILITATORS: A/Prof Philip George and Dr Shane Varman In this session, participants were divided into two groups (one with a focus on depression and another on suicide) and switched sessions after 20 minutes.
Each participant has his own way to approach these black and white films but A/Prof Rohaizan offered to guide them with a different approach – “Formulate your differential diagnoses from the summary given, and use the radiographs as a tool to refine it”. It was no easy task to adopt a new approach and the discussion was paused by a few awkward silences. However, the participants started to express their excitement as they began to appreciate the radiographs in a new light – early bronchopneumonic changes secondary to viral upper respiratory tract infection, appendicitis secondary to appendicolith causing pericolic abscess and small bowel obstruction, just to name a few. At the end of the station, the participants were exposed to radiographs of bronchopneumonia, acute laryngotracheobronchitis, acute epiglottitis, appendicitis, and intussusception. They could not hide their satisfactions after the fruitful discussion and wished to have more time to discuss more scenarios. As reported by Lim Sean Yee and Syahidah bt Mohd Noh TITLE: Assessing Depression and Suicide in Primary Care FACILITATORS: A/Prof Philip George and Dr Shane Varman In this session, participants were divided into two groups (one with a focus on depression and another on suicide) and switched sessions after 20 minutes.  Each session started off with a round of introduction. Participants were then showed a video interview and later had an interactive session where they discussed topics on history taking, investigations, diagnosis and management. For the session on depression, the patient presented with symptoms of depression (eg tiredness, loss of appetite, difficulty to concentrate etc.). The facilitator emphasised the importance of ruling out medical conditions like hypothyroidism, diabetes and anemia. It was also pointed out that in our Asian culture, patients who are depressed often present with physical symptoms rather than directly saying that they are feeling depressed. Some possible reasons included stigma associated with psychological illness and fear of being perceived as weak. In terms of history taking, it is vital to move from physical wellbeing to underlying psychological issues. Sleep, mood and appetite are the important areas to assess when taking history. It was also emphasised that primary care doctors need to pick up mild cases of depression before these patients progressed to moderate and severe depression. It was also made clear that ability to concentrate was a needed component in psychotherapy and therefore, patients who are experiencing difficulty in concentration needed to be treated with antidepressants first. For the session on suicide, a video was shown and two questions were posed to participants on what further questions they would like to ask and the suicidal risk of the patient. Risk factors and protective factors were discussed. As reported by Eunice Ann Loh TITLE: Otoscopy and Findings FACILITATORS: Dr Valu and Dr Rafiq The session is conducted in two small groups to ensure quality of training; each group containing up to 10 participants per time. Dr Valu greets the participants by showing how important it is to master otoscopy skill in managing patient in primary care setting. The reason for this is that the patient do not usually approach an ENT specialist when something mild happen, for example, ear discharge or something serious happen like a foreign body stuck in the ear. It is important for general practitioner to master the skill of otoscopy to help their patient in the near future.
Each session started off with a round of introduction. Participants were then showed a video interview and later had an interactive session where they discussed topics on history taking, investigations, diagnosis and management. For the session on depression, the patient presented with symptoms of depression (eg tiredness, loss of appetite, difficulty to concentrate etc.). The facilitator emphasised the importance of ruling out medical conditions like hypothyroidism, diabetes and anemia. It was also pointed out that in our Asian culture, patients who are depressed often present with physical symptoms rather than directly saying that they are feeling depressed. Some possible reasons included stigma associated with psychological illness and fear of being perceived as weak. In terms of history taking, it is vital to move from physical wellbeing to underlying psychological issues. Sleep, mood and appetite are the important areas to assess when taking history. It was also emphasised that primary care doctors need to pick up mild cases of depression before these patients progressed to moderate and severe depression. It was also made clear that ability to concentrate was a needed component in psychotherapy and therefore, patients who are experiencing difficulty in concentration needed to be treated with antidepressants first. For the session on suicide, a video was shown and two questions were posed to participants on what further questions they would like to ask and the suicidal risk of the patient. Risk factors and protective factors were discussed. As reported by Eunice Ann Loh TITLE: Otoscopy and Findings FACILITATORS: Dr Valu and Dr Rafiq The session is conducted in two small groups to ensure quality of training; each group containing up to 10 participants per time. Dr Valu greets the participants by showing how important it is to master otoscopy skill in managing patient in primary care setting. The reason for this is that the patient do not usually approach an ENT specialist when something mild happen, for example, ear discharge or something serious happen like a foreign body stuck in the ear. It is important for general practitioner to master the skill of otoscopy to help their patient in the near future.
Dr Rafiq started the session by showing them common mistakes made by doctors when performing otoscopy and the correct way to perform otoscopy. There were two mannequins with 13 pairs of different ear conditions in each station. Each participant was given a chance to observe each ear model with otoscopy, supervised by Dr Valu. The participant was asked to draw the findings on a plain paper. Dr. Valu corrected the technique of participants and point out the important ear condition that participants should know for example cholesteatoma because urgent referral is needed. Participants were given chance to discuss common ENT problems. Dr Valu discussed tympanoplasty and mastoidectomy in detail. In conclusion, Dr Valu mentioned that a proper ENT assessment for each patient is essential and proper technique is required to recognise serious ENT disorder for early intervention. As reported by Chua Chen Zhi TITLE: Evaluation of common medical problems and ECG FACILITATORS: Dr Anis Ahmed Khan and Team This is a workshop focusing mainly on common clinical presentation of patients with positive findings on the electrocardiogram. Participants were given 8 scenarios over a period of 40 minutes or 5 minutes for each scenario, consisting of a brief summary of the respective medical condition, an ECG and several questions on the appropriate investigation and management. These were shown on PowerPoint slides and participants were expected to actively involve themselves in the discussion especially during the interpretation of ECG.
 Some medical problems such as pulmonary embolism, junctional escape beat, 3rd degree heart block, Wolff-Parkinson-White syndrome and ventricular tachycardia were discussed. Since there were 5 groups of participants, each consisting of 20 participants at the most, each session of 40 minutes was conducted by different lecturers. At the final 5 to 10 minutes of each session, the lecturer would open the floor for questions. However, there was not much of an active discussion. This could be due to the lack of time for the participants to interpret the ECG especially when a number of participants were made up of medical students. Due to time constraints and the number of scenarios, time was insufficient for discussions.
Some medical problems such as pulmonary embolism, junctional escape beat, 3rd degree heart block, Wolff-Parkinson-White syndrome and ventricular tachycardia were discussed. Since there were 5 groups of participants, each consisting of 20 participants at the most, each session of 40 minutes was conducted by different lecturers. At the final 5 to 10 minutes of each session, the lecturer would open the floor for questions. However, there was not much of an active discussion. This could be due to the lack of time for the participants to interpret the ECG especially when a number of participants were made up of medical students. Due to time constraints and the number of scenarios, time was insufficient for discussions.
Overall, the workshop went smoothly and time management was good. As reported by Chan Yi-Min Main Conference Day 2 – 27 September 2014 TITLE: Osteoarthritic Knees SPEAKER: Dr Nayyer Naveed Wazir Osteoarthritis is a degenerative joint disorder commonly seen in elderly populations, especially among women. Knee joints are among the articulations frequently involved. This debilitating disease is mechanical in nature, in which patients typically experience more pain upon standing and movement, vice versa when at rest. The deformities are also better appreciated when the radiograph is taken with the patient standing. Although one can make a diagnosis of osteoarthritis by looking for its typical radiological signs, a good history is irreplaceable. Various sophisticated disease modifying agents, such as hyaluronic injections, arthroscopic debridement, and joint replacements; has been used in managing the disease.  Being among the commonly used, hyaluronic injections can be done in the office and requires strict asepsis. It may induce hypersensitivity or flare up local inflammation, and infection, if aseptic technique is not practiced. It is recommended to give once a week for 3 to 5 consecutive weeks through a 22G or 23G needle under local anaesthesia. The drug should be kept at 1 to 30°C and should be allowed to return to room temperature before injection. Despite all the exciting choices of therapy, the quadriceps-strengthening exercise, hamstrings-strengthening exercises, and off-loading of joint are compulsory for all patients. As reported by Lim Sean Yee TITLE: Evaluating Women with Urinary Incontinence SPEAKER: A/Prof Sharifah Suhaila The speaker chose this topic as it is one of the commonest complaints among women. Urinary incontinence was defined as involuntary urine loss, which is sufficient to give rise to social, and hygiene problem. It can be divided into a few types, namely overactive bladder, overflow incontinence and stress incontinence. Patients with this condition will experience symptoms such as frequent intense urge to urinate that cannot be voluntarily suppressed, leakage at coughing or laughing, nocturnal wetting and intact or diminished perineal sensation.’
Being among the commonly used, hyaluronic injections can be done in the office and requires strict asepsis. It may induce hypersensitivity or flare up local inflammation, and infection, if aseptic technique is not practiced. It is recommended to give once a week for 3 to 5 consecutive weeks through a 22G or 23G needle under local anaesthesia. The drug should be kept at 1 to 30°C and should be allowed to return to room temperature before injection. Despite all the exciting choices of therapy, the quadriceps-strengthening exercise, hamstrings-strengthening exercises, and off-loading of joint are compulsory for all patients. As reported by Lim Sean Yee TITLE: Evaluating Women with Urinary Incontinence SPEAKER: A/Prof Sharifah Suhaila The speaker chose this topic as it is one of the commonest complaints among women. Urinary incontinence was defined as involuntary urine loss, which is sufficient to give rise to social, and hygiene problem. It can be divided into a few types, namely overactive bladder, overflow incontinence and stress incontinence. Patients with this condition will experience symptoms such as frequent intense urge to urinate that cannot be voluntarily suppressed, leakage at coughing or laughing, nocturnal wetting and intact or diminished perineal sensation.’  “What are the causes of urinary incontinence?” The speaker explained that common causes include over activity of detrusor muscle due to myogenic, neurogenic or idiopathic factors, insulin dependent diabetes, anatomical defect of bladder and weakness of pelvic floor. It can also be due to trauma to lumbar spine and prolapsed disc. The key to evaluation of urinary incontinence is to make the correct diagnosis and eliminate other causes, look for associated problems, know the patient’s profile, examine her thoroughly, carry out effective tests and provide treatment options. Urodynamic evaluation and pelvic examinations such as Q tip test, Bonney’s test and pelvic floor examination can be done as well. Patients are advised to keep a Voiding Diary to assess their progress.The speaker ended her speech by explaining treatment of urinary incontinence. The choices include non-surgical option or pharmacotherapy and surgical treatment. As reported by Soh Wan Wen TITLE: Suturing – Tips and Tricks SPEAKER: Prof Lum Siew Kheong
“What are the causes of urinary incontinence?” The speaker explained that common causes include over activity of detrusor muscle due to myogenic, neurogenic or idiopathic factors, insulin dependent diabetes, anatomical defect of bladder and weakness of pelvic floor. It can also be due to trauma to lumbar spine and prolapsed disc. The key to evaluation of urinary incontinence is to make the correct diagnosis and eliminate other causes, look for associated problems, know the patient’s profile, examine her thoroughly, carry out effective tests and provide treatment options. Urodynamic evaluation and pelvic examinations such as Q tip test, Bonney’s test and pelvic floor examination can be done as well. Patients are advised to keep a Voiding Diary to assess their progress.The speaker ended her speech by explaining treatment of urinary incontinence. The choices include non-surgical option or pharmacotherapy and surgical treatment. As reported by Soh Wan Wen TITLE: Suturing – Tips and Tricks SPEAKER: Prof Lum Siew Kheong 
Suturing is an essential skill that has to be mastered by medical practitioners for emergency and trauma. Thus, this slot was particularly important in facilitating a better understanding and approach to the skill. There were five important elements; namely the purpose of suturing; choice of needles and sutures; an introduction to the Langer’s Lines to improve the cosmetic outcome; and what sort of tricks could be used during special situations. It was clear that suturing is essential in the prevention of infection which further provides a good cosmetic result. This facilitates patient’s adaptation post-trauma.
Specific suture materials were also introduced to ensure practitioners would choose the right materials for the right lacerations. In conclusion, Prof Lum managed to illustrate the differences that better suturing techniques can contribute to improving patient’s quality of life. As reported by Reena Priya TITLE: Paediatric Emergency SPEAKER: A/Prof Stefan Kutzche The main objective of this talk was to re-visit and sharpen the basic skills in dealing with pediatric emergency. It is important to take note that children are not small adults. The unique anatomical and physiological features of children require special consideration in assessment and management. During the talk, Advanced Pediatric Life Support (APLS) which is a programme created by the American Academy of Pediatrics and the American College of Emergency Physicians was introduced to the participants on how to assess and manage sick children during an emergency. The pediatric assessment triangle is one of the core components of the APLS.  Assessment of a sick child is based on a quick examination of their appearance, breathing, and circulation. The appearance is determined by an examination of tone, how interactive the child is and if they are consolable. Their gaze and the quality of their speech or cry are also observed. On the other hand, the work of breathing is determined by the presence of abnormal airways sounds, abnormal positioning, retractions, nasal flaring and head bobbing. Last but not least, general inspection of the presence of pallor, mottling and cyanosis are assessed to determine the circulation to skin. A few scenarios were given and the discussion of the scenarios mainly focused on the approach and management in different cases. As reported by Lim Fang Chan TITLE: Clinical Approach to the Red Eye SPEAKER: Dr Puneet Agarwal
Assessment of a sick child is based on a quick examination of their appearance, breathing, and circulation. The appearance is determined by an examination of tone, how interactive the child is and if they are consolable. Their gaze and the quality of their speech or cry are also observed. On the other hand, the work of breathing is determined by the presence of abnormal airways sounds, abnormal positioning, retractions, nasal flaring and head bobbing. Last but not least, general inspection of the presence of pallor, mottling and cyanosis are assessed to determine the circulation to skin. A few scenarios were given and the discussion of the scenarios mainly focused on the approach and management in different cases. As reported by Lim Fang Chan TITLE: Clinical Approach to the Red Eye SPEAKER: Dr Puneet Agarwal  The aim of the talk was to understand and clinically manage the red eye in patients. The aim of the speaker was to highlight the common presenting symptom of many ophthalmic disease, to differentiate acute and chronic manifestations of ophthalmic diseases, understand the variable severity of these diseases, differentiate the different causation of unilateral and bilateral manifestations of ophthalmic diseases as well as differentiate and understand the infectious, allergic, autoimmune, inflammatory and traumatic causes of ophthalmic diseases. The speaker also spoke about the key points in the managements of ophthalmic diseases by identifying cases with underlying ophthalmic causes and how to manage them. The speaker provided a very thorough explanation on the pathophysiology of conjunctival and ciliary injection, the common clinical history, physical findings, examination method, differential diagnosis of red eyes in patients. Some of the ophthalmologic conditions were conjunctivitis, episcleritis, subconjunctival haemorrhage, foreign objects, corneal abrasion, infections of the cornea (considered an opthlamologic emergency), corneal ulcers, scleritis, anterior uveitis and glaucoma. Red eye is currently one of the most common complaint. Although most of the cases are benign and self-limiting, doctors must never forget to look for “Red Flags” in order to detect dangerous ophthalmic conditions. As reported by Aslinah Binti Velayit Hussein Clinical Skills – Hands-on TITLE: Debridement and Suturing Skills FACILITATOR: Prof Lum Siew Kheong & Department of Surgery colleagues
The aim of the talk was to understand and clinically manage the red eye in patients. The aim of the speaker was to highlight the common presenting symptom of many ophthalmic disease, to differentiate acute and chronic manifestations of ophthalmic diseases, understand the variable severity of these diseases, differentiate the different causation of unilateral and bilateral manifestations of ophthalmic diseases as well as differentiate and understand the infectious, allergic, autoimmune, inflammatory and traumatic causes of ophthalmic diseases. The speaker also spoke about the key points in the managements of ophthalmic diseases by identifying cases with underlying ophthalmic causes and how to manage them. The speaker provided a very thorough explanation on the pathophysiology of conjunctival and ciliary injection, the common clinical history, physical findings, examination method, differential diagnosis of red eyes in patients. Some of the ophthalmologic conditions were conjunctivitis, episcleritis, subconjunctival haemorrhage, foreign objects, corneal abrasion, infections of the cornea (considered an opthlamologic emergency), corneal ulcers, scleritis, anterior uveitis and glaucoma. Red eye is currently one of the most common complaint. Although most of the cases are benign and self-limiting, doctors must never forget to look for “Red Flags” in order to detect dangerous ophthalmic conditions. As reported by Aslinah Binti Velayit Hussein Clinical Skills – Hands-on TITLE: Debridement and Suturing Skills FACILITATOR: Prof Lum Siew Kheong & Department of Surgery colleagues  The participants were introduced to different types of sutures; namely absorbable, non-absorbable and the different situations they are used for. Different types of needles were discussed, namely, cutting, reverse cutting and round body needles. The participants were then taught principles on wound debridement. They were taught that wounds must be cleaned but it was not necessary to make them sterile. The participants then actively irrigated the soiled wounds on chicken drumsticks with the solutions provided. Finally, they were taught four different types of suturing – interrupted, continuous, vertical mattress and horizontal mattress. Some sutured on the chicken drumstick while others used the chicken skin. The facilitators divided themselves and helped each small group. While guiding the participants, they also shared their experiences from their clinical practice. The station was set up on two sides. While one side was in operation, the volunteers prepared the other side for the next group of participants. All in all, the participants enjoyed the station very much and learnt a lot. It was a great privilege to learn from the various surgeons and glean from their vast experiences and exposure. As reported by Eunice Ann Loh TITLE: Interpretation of Investigations and Formulating Diagnostic Approach in Women with Urinary Incontinence FACILITATORS: Dr Kavitha Nagandla, Dr Bheena Vyshali and Dr Hussein Akl
The participants were introduced to different types of sutures; namely absorbable, non-absorbable and the different situations they are used for. Different types of needles were discussed, namely, cutting, reverse cutting and round body needles. The participants were then taught principles on wound debridement. They were taught that wounds must be cleaned but it was not necessary to make them sterile. The participants then actively irrigated the soiled wounds on chicken drumsticks with the solutions provided. Finally, they were taught four different types of suturing – interrupted, continuous, vertical mattress and horizontal mattress. Some sutured on the chicken drumstick while others used the chicken skin. The facilitators divided themselves and helped each small group. While guiding the participants, they also shared their experiences from their clinical practice. The station was set up on two sides. While one side was in operation, the volunteers prepared the other side for the next group of participants. All in all, the participants enjoyed the station very much and learnt a lot. It was a great privilege to learn from the various surgeons and glean from their vast experiences and exposure. As reported by Eunice Ann Loh TITLE: Interpretation of Investigations and Formulating Diagnostic Approach in Women with Urinary Incontinence FACILITATORS: Dr Kavitha Nagandla, Dr Bheena Vyshali and Dr Hussein Akl  To begin with, introduction about the station was given by facilitators from Department of Obstetrics and Gynecologist. One of them was Dr Kavitha Nagandla and she was helped by Dr Bheena Vyshali and Dr Hussein Akl. There were 5 groups of participants. Basically, this station started with a role-play between a participant and the simulated patient which involved history taking, and patient counseling. There were also participants who volunteered to discuss about the examination that they wanted to do, and some interpretations of urine analysis. In between the role play, there were some discussions done by the facilitators. In conclusion, this station was an interactive and meaningful station where it involved the participants to do role-play. At the end of the session, most of the participants were satisfied with the knowledge and hopefully they can apply it in their practice. As reported by Lim Sean Yee and Syahidah bt Mohd Noh TITLE: Joint aspiration and injection FACILITATOR: Prof Naveed, Prof Kareem and Dr Surinder This is a real case station where 14 patients benefited from the treatment. 14 patients with osteoarthritis were invited for this station as real patients for performing joint injection technique. Prof Naveed introduced the topic of joint aspiration and the clinical indication of doing it. Then, Prof Naveed taught participants how to locate the anatomical position of the joint space with the knee flexed. The injection spot was above the lateral condyle of tibia bone. The injection spot was marked using marker pen.
To begin with, introduction about the station was given by facilitators from Department of Obstetrics and Gynecologist. One of them was Dr Kavitha Nagandla and she was helped by Dr Bheena Vyshali and Dr Hussein Akl. There were 5 groups of participants. Basically, this station started with a role-play between a participant and the simulated patient which involved history taking, and patient counseling. There were also participants who volunteered to discuss about the examination that they wanted to do, and some interpretations of urine analysis. In between the role play, there were some discussions done by the facilitators. In conclusion, this station was an interactive and meaningful station where it involved the participants to do role-play. At the end of the session, most of the participants were satisfied with the knowledge and hopefully they can apply it in their practice. As reported by Lim Sean Yee and Syahidah bt Mohd Noh TITLE: Joint aspiration and injection FACILITATOR: Prof Naveed, Prof Kareem and Dr Surinder This is a real case station where 14 patients benefited from the treatment. 14 patients with osteoarthritis were invited for this station as real patients for performing joint injection technique. Prof Naveed introduced the topic of joint aspiration and the clinical indication of doing it. Then, Prof Naveed taught participants how to locate the anatomical position of the joint space with the knee flexed. The injection spot was above the lateral condyle of tibia bone. The injection spot was marked using marker pen.  Before the procedure, Prof Naveed assessed patient current complaint and performed full clinical examination for the patient. Following that, sterile technique was performed during the procedure. With the help of the volunteers, Prof Naveed cleaned the patient’s leg using Povidone. Injection of sodium hyaluronic acid was given through the injection spot of the patient. Prof Naveed clearly stated the angle, depth and possible complication of the procedure. Some of the participants were able to perform the injection technique under the supervision of Dr Surinder. Prof Naveed mentioned the importance of weight bearing exercise to the patient after procedure is done. In conclusion, Prof Naveed mentioned that the current procedure is strictly sterile procedure because if we introduce bacteria inside the joint of the patient, it will be chronic osteomyelitis which will be the nightmare of both doctors and patients. As reported by Chua Chen Zhi TITLE: Mock “Code Blue” in Paediatrics FACILITATOR: A/Prof Stefan and Team This workshop mainly focused on recognising and managing paediatric emergencies. In this station, two different scenarios were given; septic shock in an infant and cardiac arrest in a child. Prof Stephan and Dr Erwin were in charge of the septic shock scenario whereas Dr Kyin Win and Dr Ng were in charge for the cardiac arrest scenario. There were two streams going on simultaneously, and two stations (septic shock and cardiac arrest) in each stream. After 20 minutes, the participants swapped streams. At the end of each stream, participants proceeded to the hands-on session for setting an intra-osseous line using chicken drumsticks. They were guided by Dr San, Dr Erwin and Prof Stefan. At the cardiac arrest station, two arrhythmias were given: asystole and ventricular fibrillations. The participants were expected to perform CPR and defibrillate according to the American Paediatrics Life Support Protocol. As for the septic shock station, the delegates needed to provide adequate oxygen and fluid resuscitation and identify the source of shock and treat accordingly. Blood pressure should also be controlled with vasoactive drugs such as dopamine and adrenaline when necessary.
Before the procedure, Prof Naveed assessed patient current complaint and performed full clinical examination for the patient. Following that, sterile technique was performed during the procedure. With the help of the volunteers, Prof Naveed cleaned the patient’s leg using Povidone. Injection of sodium hyaluronic acid was given through the injection spot of the patient. Prof Naveed clearly stated the angle, depth and possible complication of the procedure. Some of the participants were able to perform the injection technique under the supervision of Dr Surinder. Prof Naveed mentioned the importance of weight bearing exercise to the patient after procedure is done. In conclusion, Prof Naveed mentioned that the current procedure is strictly sterile procedure because if we introduce bacteria inside the joint of the patient, it will be chronic osteomyelitis which will be the nightmare of both doctors and patients. As reported by Chua Chen Zhi TITLE: Mock “Code Blue” in Paediatrics FACILITATOR: A/Prof Stefan and Team This workshop mainly focused on recognising and managing paediatric emergencies. In this station, two different scenarios were given; septic shock in an infant and cardiac arrest in a child. Prof Stephan and Dr Erwin were in charge of the septic shock scenario whereas Dr Kyin Win and Dr Ng were in charge for the cardiac arrest scenario. There were two streams going on simultaneously, and two stations (septic shock and cardiac arrest) in each stream. After 20 minutes, the participants swapped streams. At the end of each stream, participants proceeded to the hands-on session for setting an intra-osseous line using chicken drumsticks. They were guided by Dr San, Dr Erwin and Prof Stefan. At the cardiac arrest station, two arrhythmias were given: asystole and ventricular fibrillations. The participants were expected to perform CPR and defibrillate according to the American Paediatrics Life Support Protocol. As for the septic shock station, the delegates needed to provide adequate oxygen and fluid resuscitation and identify the source of shock and treat accordingly. Blood pressure should also be controlled with vasoactive drugs such as dopamine and adrenaline when necessary. 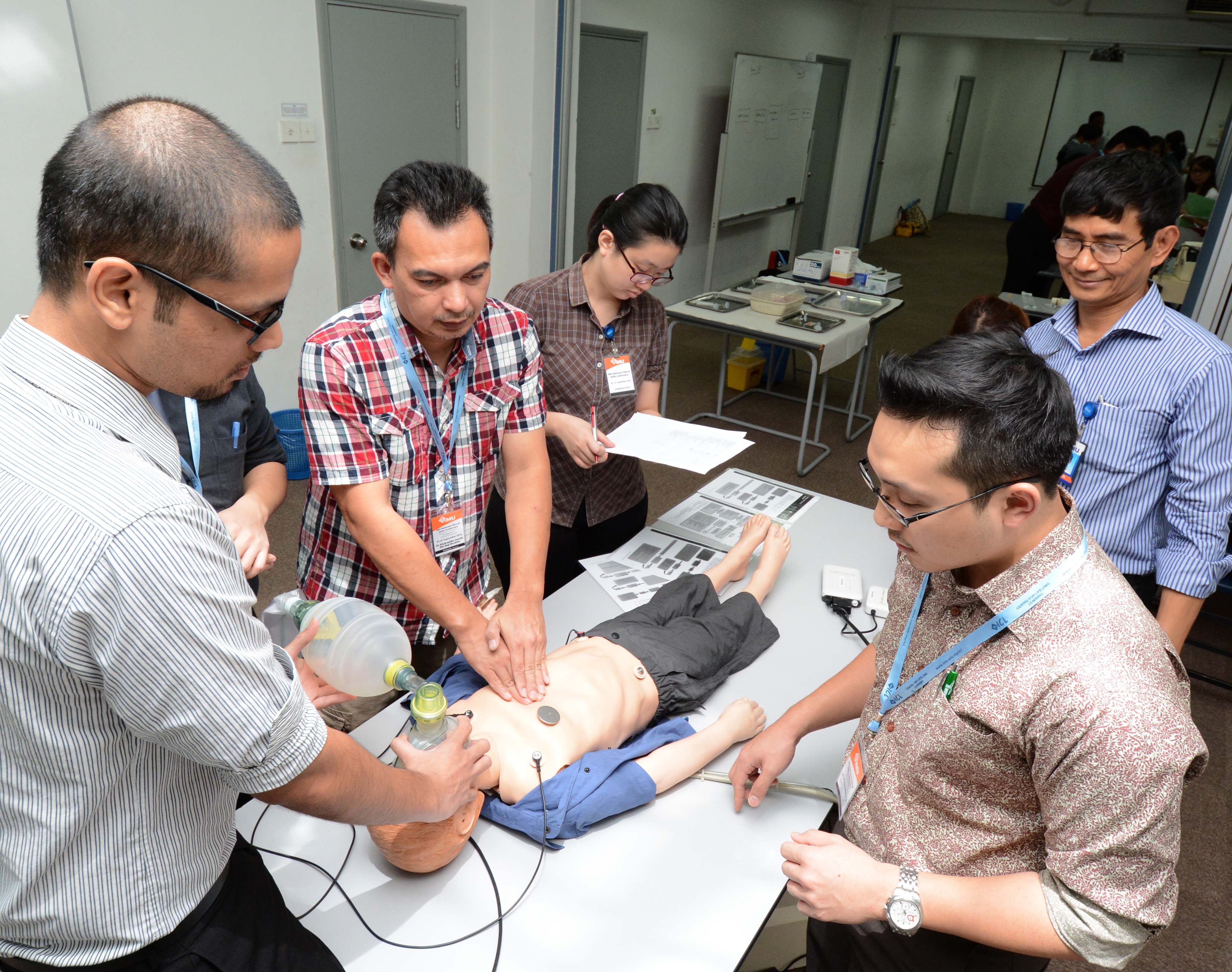 In general, the teamwork varied from group to group. This was mainly due to the fact that they were not familiar with each other, also because some team leaders were not really familiar with the code blue activation and paediatric resuscitation. The lack of close loop communications had resulted in a quiet and an inactive resuscitation. In most of the scenarios, due to improper management, the child / infant died or sustained a hypoxic ischemic encephalopathy. Paediatric Emergencies can be fatal and every doctor should know how to manage them appropriately. Time management was an issue, because the first group and the third group that came after tea break were late, resulting in a 5-10 minutes delay. Although this was a simulated station, some of the equipment were not present and had to be retrieved from the hospital and store room. In conclusion, Paediatrics Code Blue generally received good feedback, the facilitators and student helpers were all very helpful, if we can make the simulation more realistic it would have a greater effect in terms of creating the settings or urgency and emergency. As reported by Celina Choo TITLE: Fundoscopy using Pan Optic Opthalmoscope with Smartphone Attachment FACILITATOR: Dr Puneet
In general, the teamwork varied from group to group. This was mainly due to the fact that they were not familiar with each other, also because some team leaders were not really familiar with the code blue activation and paediatric resuscitation. The lack of close loop communications had resulted in a quiet and an inactive resuscitation. In most of the scenarios, due to improper management, the child / infant died or sustained a hypoxic ischemic encephalopathy. Paediatric Emergencies can be fatal and every doctor should know how to manage them appropriately. Time management was an issue, because the first group and the third group that came after tea break were late, resulting in a 5-10 minutes delay. Although this was a simulated station, some of the equipment were not present and had to be retrieved from the hospital and store room. In conclusion, Paediatrics Code Blue generally received good feedback, the facilitators and student helpers were all very helpful, if we can make the simulation more realistic it would have a greater effect in terms of creating the settings or urgency and emergency. As reported by Celina Choo TITLE: Fundoscopy using Pan Optic Opthalmoscope with Smartphone Attachment FACILITATOR: Dr Puneet  The objective of this workshop was to provide hands-on skills for participants on different techniques of ophthalmoscopy in order to detect any abnormalities of the eyes. The direct ophthalmoscope is the instrument of choice for fundus examination by medical students and physicians but through panoptic ophthalmoscope, it allows for a magnified, monocular image of the retina and optic disc. Welch Allyn PanOptic Ophthalmoscope provides fast, easy entry into small non-dilated pupils, a 5x larger view of the fundus than with a standard ophthalmoscope and a 25 degree Field of View, a four-fold increase in magnification, making it easier to see retinal details. Annals of Family Medicine now recommend this as the best for screening diabetic retinopathy. The design of the Welch Allyn PanOptic also allows for a greater working distance between the practitioner and patient, improving comfort for both as it makes it easy to enter small non-dilated eyes. Two simulated patients were there for practice purposes. The session concluded with discussions and practical self-practice sessions on fundoscopy. As reported by Adrian Lee Huan Han
The objective of this workshop was to provide hands-on skills for participants on different techniques of ophthalmoscopy in order to detect any abnormalities of the eyes. The direct ophthalmoscope is the instrument of choice for fundus examination by medical students and physicians but through panoptic ophthalmoscope, it allows for a magnified, monocular image of the retina and optic disc. Welch Allyn PanOptic Ophthalmoscope provides fast, easy entry into small non-dilated pupils, a 5x larger view of the fundus than with a standard ophthalmoscope and a 25 degree Field of View, a four-fold increase in magnification, making it easier to see retinal details. Annals of Family Medicine now recommend this as the best for screening diabetic retinopathy. The design of the Welch Allyn PanOptic also allows for a greater working distance between the practitioner and patient, improving comfort for both as it makes it easy to enter small non-dilated eyes. Two simulated patients were there for practice purposes. The session concluded with discussions and practical self-practice sessions on fundoscopy. As reported by Adrian Lee Huan Han