• Testicular cancer is the most common cancer in men aged 15-34. • In Malaysia, testicular cancer is the 9th and 10th most frequent cancers in males aged 0-14 years old and 14-49 years old. Majority of them were of Malay ethnicity. The average age at presentation was 33.7 years. • There are two main types of testicular cancers: seminoma and non-seminoma. • The first symptom of testicular cancer is a painless lump or swelling in the scrotum. • The most common sites of spread for testicular cancer are the lymph nodes in the back of the abdomen, called the retroperitoneal lymph nodes. • Testicular cancers are very sensitive to chemotherapy and are curable even when metastatic (spread of the cancer cells in distant sites). What is Testis? 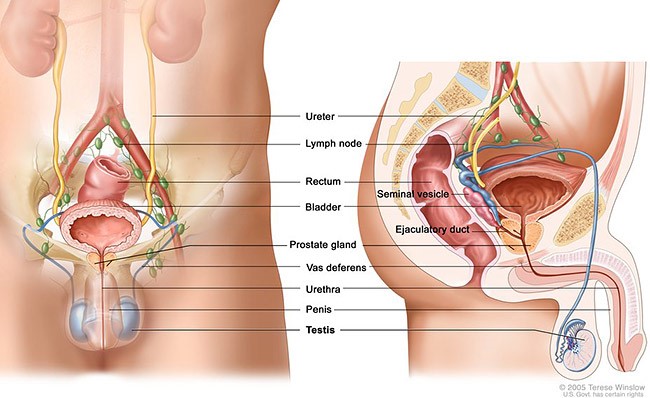
Figure 1: Male reproductive system
• Testes are paired of oval glands located within the scrotum. • They are the male reproductive organs which produced sperm and sex hormones. • Most testicular cancer arises from the germ cells (reproductive cells), and rarely the non–germ cell tumors which arise from Leydig or Sertoli cells.
What are the Risk Factors for Testicular Cancer? • Congenital malformations of the male genitalia – Cryptorchidism (undescended testis) • Family history of testicular cancer Activities such as horseback or motorcycle riding, local trauma and increased scrotal temperature have not been associated with increased risk of testicular cancer. What are the Signs and Symptoms? Early presentations: • Painless swelling of one testis which is noted incidentally • Dull ache or heavy sensation in the lower abdomen, perianal area or scrotum • Sudden onset of pain in the testis or scrotum • Groin mass Late presentations: • Neck mass (spread to lymph node) • Cough or dyspnea (spread to lungs) • Anorexia, nausea, vomiting, or gastrointestinal bleeding • Bone pain (spread to bone) Differentiation of testicular cancer from other testicular swelling: • Testicular cancer: solid, firm to hard mass and may be painless or painful • Hernia: expands upon coughing and reducible on direct pressure or when lying down • Hydrocele: may be huge but painless and contain large amount of fluid How is Testicular Cancer Diagnosed? Diagnostic evaluation of suspected testicular cancer include: • Testicular ultrasound: This is an imaging test that creates pictures of the inside of the testis and can show abnormal growths. • CT scan, PET scan of the abdomen and pelvis: To look for the extent of the cancer spread in the body. • Serum tumor markers (alpha fetoprotein, beta-hCG, LDH): To help in diagnosis and evaluate the outcome of testicular cancer. • Radical inguinal orchiectomy (removal of testis): To confirm the diagnosis of testicular cancer and provide local tumor control. • Retroperitoneal lymph node removal: To identify the spread to lymph nodes and provide accurate staging. How is Testicular Cancer Treated? The need for further treatment depends on: • Type of cancer • The stage of the cancer • The prognosis Treatment options: • Surgery • Chemotherapy • Radiotherapy • Combination of surgery, chemotherapy and radiation therapy can improve the chances of curing the cancer Surgery – Radical inguinal orchiectomy (removing the affected testis) is first step in treatment. During the surgery, the entire testicle is usually removed to avoid the risk of spreading the tumor within the scrotum. Testicular cancer is sometimes treated with surgery to remove nearby lymph nodes and also other part of the body to prevent the spread of testicular cancer in the body. Chemotherapy – Chemotherapy is the term doctors use to describe a group of medicines that stop or slow the growth of cancer cells. Chemotherapy works by interfering with the ability of rapidly growing cells (like cancer cells) to divide or multiply. A few cycle of chemotherapy is necessary to stop the growth of the cancer cells. Side effects of chemotherapy: Fatigue, hair loss, nausea and vomiting are not uncommon. Long term complications include kidney damage, nerve damage, pain in the arms and feet, hearing loss, damage to blood vessels in the heart and potential of increasing the risk of cardiovascular disease, and lung scarring. This typically occurs many years after treatment is completed. Radiation therapy – Radiation therapy (RT) refers to the exposure of a tumor to high-energy X-rays in order to slow or stop its growth. Exposure to X-rays damages cells. Unlike normal cells, cancer cells cannot repair the damage caused by exposure to X-rays, particularly when it is administered over several days. This prevents the cancer cells from growing further and causes them to eventually die. However, there are potential risks of RT, including impaired fertility, second malignancy or late heart disease. For these reasons, RT is usually reserved for older men, men who could not tolerate chemotherapy, and men who are not good candidates for surveillance. Other side effects include gastrointestinal effects such as nausea, vomiting, increased stool frequency and rapid gastric emptying. Active Surveillance (rigorous follow-up schedule) – In some cases, men with small Stage I testicular cancers do not require more treatment after orchiectomy. However, these men need regular follow-up with a healthcare provider to monitor for signs of relapse. This approach is called surveillance. During surveillance, you will be seen every few months for a physical examination, blood tests, and imaging studies (eg, CT scan of the abdomen and pelvis, chest X-ray). This schedule is recommended for the first three to four years, and then visits may become less frequent (eg, twice per year for several years, and then once per year until at least 10 years after diagnosis). What is the Prognosis after Treatment? Prognosis is the chance that a patient will recover or have a recurrence (return of the cancer). Many factors can affect a person’s prognosis, including: • The type and location of the cancer • The stage of the disease (the extent to which the cancer has metastasised or spread) • Its grade (how abnormal the cancer cells look and how quickly the cancer is likely to grow and spread) • The person’s age, general health, and response to treatment. Men with Stage I disease have an excellent chance for cure when treated appropriately. Patients who have an intermediate or poor prognosis also generally respond well to treatment and require a more aggressive treatment regimen. Even for those with a poor prognosis, approximately half can be cured. Prepared by: Prof Ariyananda, Department of Internal Medicine, Clinical School Seremban, International Medical University Liew Kai Hsiang, Semester 9 Students, International Medical University Chioh Ling Shyan, Semester 9 Students, International Medical University Choy Shet Yee, Semester 9 Students, International Medical University Velentine Anderson, Semester 9 Students, International Medical University Nancy , Deanery, Clinical School Seremban, International Medical University









