| What is osteoporosis? |
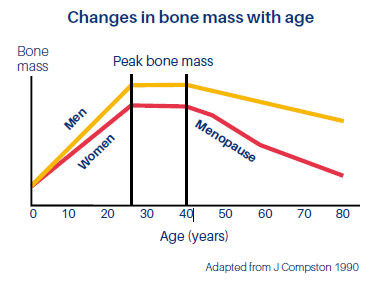
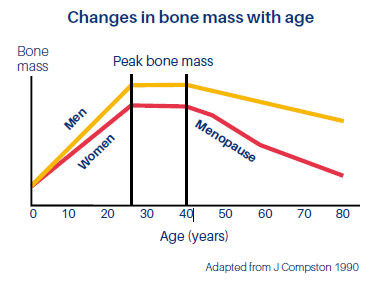
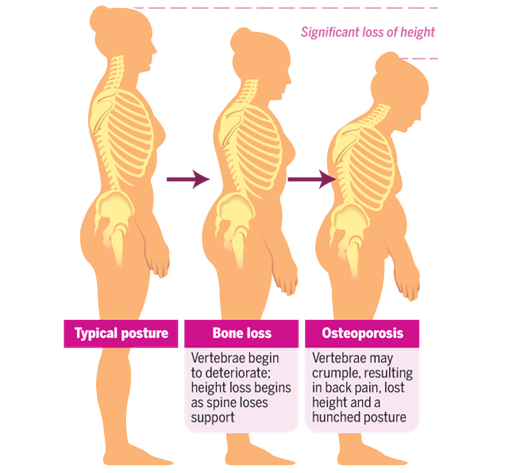
| Osteoporosis means spongy (porous) bone. Osteoporosis is a condition where there is “thinning” of the bones and that affects bone strength (the word osteoporosis literally means “porous bones”). Bone is made of tough, elastic fibres (collagen fibres) and gritty, hard material (minerals). In childhood and adolescence, new bone is formed very quickly. But, as we get older, this reverses. As a result, from about the age of 35, we start to lose a certain amount of bone material overall and the bones become less dense and less strong. |
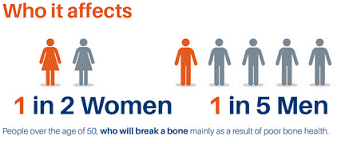
| How common is osteoporosis? |
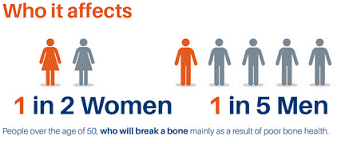
| Osteoporosis is common and it shows an increasing trend worldwide. At the age of 50, about 2 in 100 women have osteoporosis. This rises to 1 in 4 women at the age of 80. But, osteoporosis can also affect men. About 54 million people are affected by osteoporosis in the United States. |
| Who is at increased risk for osteoporosis? |
| Key risk factors for osteoporosis include: • Family history: Osteoporosis seems to run in families. If your mother had a hip fracture or spinal collapse fracture, chances are you are at risk for osteoporosis. • Gender: Women are four times more likely than men to get osteoporosis. But men also suffer from osteoporosis. • Age: The risk of osteoporosis increases with age. Women over age 50 have the greatest risk of developing osteoporosis. • Bone structure and body weight: Petite and thin women have a greater risk of developing osteoporosis. People with BMI < 19 are at risk. • History of fractures: Having one fracture increases the chance of more fractures. • Smoking: Smoking increases the risk of fractures. Studies show that cigarette smokers (past or current smokers) have lower bone densities and higher fracture risks. Women who smoke have lower levels of estrogen. • Medications: Some medications may increase your risk of osteoporosis. These include long-term use of steroids (prednisone), thyroid drugs, anticonvulsants, antacids, and other drugs.. • Early menopause before the age of 45. |
| Other factors include: • Lack calcium and/or vitamin D (due to a poor diet and/or little exposure to sunlight). • Lack of weight-bearing exercise • Immobility. For example if the patient is confined to a bed or chair and unable to get about. |
| Some other medical conditions add to the risk of osteoporosis. For example: • An overactive thyroid, • Chronic kidney disease. • Rheumatoid arthritis. • Chronic liver disease. • Type 1 diabetes. • Any condition that causes poor mobility. • Many more |
| Signs & Symptoms of Osteoporosis |
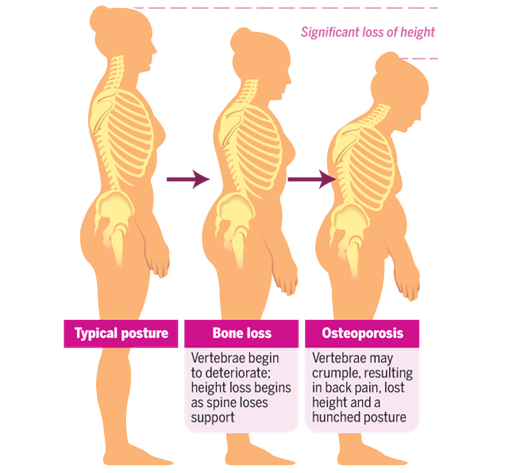
| • May be asymptomatic. • Fracture after a minor fall or a sudden impact causes a bone fracture. • Silent spine fracture may present with back pain. • When osteoporosis gets worse, even a cough or sneeze can cause a rib fracture or the partial collapse of one of the bones of the spine. • With the deformity due to the fractures, one can have a stooped posture and loss of height over time. |
| Prevention of osteoporosis |
| The ideal situation is that ‘thinning’ of the bones (osteoporosis) should be prevented in the first place.The following may help to prevent, or slow down, bone loss. Exercise: The pulling and tugging on the bones by the muscles during exercise helps to stimulate bone-making cells and strengthens the bones. Weight-bearing exercise and muscle strengthening exercises are recommended. Although mild exercise does not protect bones, moderate exercise (more than 3 days a week for more than a total of 90 minutes a week) reduces the risk for osteoporosis and fracture in both older men and women. What type of exercises are beneficial? |
| • Climbing stairs • Dancing • Jogging • Racquet sports • Running |
• Tai chi • Walking • Water aerobics • Yoga |
|
Before beginning any strenuous exercise programme, older patients or those who have serious medical conditions should talk to their doctors. Weight-bearing exercise applies tension to muscle and bone and, in young people, can increase bone density by as much as 2 – 8% a year. Food and diet: Calcium and Vitamin D are important for bone health. Therefore drinking milk, eating 50 g (2 oz) of hard cheese such as Cheddar or Edam, or one pot of yoghurt (125 g), or 50 g of sardines can provide enough calcium to the body. Vitamin D: Exposure to morning sun is good for production of Vitamin D and eating cooked salmon or cooked mackerel or tuna also helps to increase it. Going outside for 10 minutes in the midday sun—in shorts and a tank top with no sunscreen—will give you enough radiation to produce about 10,000 international units units of the Vitamin D. Stop smoking. Reduce alcohol intake. Preventing falls and fractures An important component in reducing the risk for fractures is preventing falls. Causes of fall in elderly:
- Balance and gait: As we age, most of us lose some coordination, flexibility, and balance— primarily through inactivity, making it easier to fall.
- Vision: In the aging eye, less light reaches the retina—making contrasting edges, tripping hazards, and obstacles harder to see.
- Medications: Some prescriptions and over-the-counter medications can cause dizziness, dehydration or interactions with each other that can lead to a fall.
- Environment: Most seniors have lived in their homes for a long time and have never thought about simple modifications that might keep it safer as they age.
- Chronic conditions: More than 90% of older adults have at least one chronic condition like diabetes, stroke, or arthritis. Often, these increase the risk of falling because they result in lost function, inactivity, depression, pain, or multiple medications.
Recommendations for preventing falls or fractures from falls in elderly people include:
| 1. Have proper footwear. 3. Controlling intake of certain medications (such as tranquilizers and sleeping pills) 5. Exercise to maintain strength and balance if there are no conflicting medical conditions. 7. Do not use loose rugs on the floors |
2. Move any obstructions to walking, such as loose cords or very low pieces of furniture, away from travelled areas. 4. Rooms should be well lit. 6. Have regular eye check-up. 8. Consider installing grab bars in bathrooms especially near shower, tub, or toilet. |
|
| How is osteoporosis diagnosed? |
| Osteoporosis Self-Assessment Tool for Asians (OSTA) is a simple screening tool that was developed for postmenopausal Asian women and it is based on age and weight.If the patient is found to be at increased risk, or the risk is uncertain, he may be referred for a DEXA scan. DEXA stands for dual-energy X-ray absorptiometry. It is a scan that uses special X-ray machines to check the bone density. |
| How useful is DEXA? |
| BMD (Bone Mineral Density) is the gold standard to diagnose osteoporosis in Malaysia. |
| What will the results tell me? |
The BMD test results are compared to that of a healthy 30-year-old adult, and the results are given as T-score. A T-score between +1 and −1 is considered normal or healthy between −1 and −2.5 indicates that you have low bone mass (osteopenia), although not low enough to be diagnosed with osteoporosis. A T-score of −2.5 or lower indicates that you have osteoporosis. |
| Who should be screened for osteoporosis? |
| 1. All women above 65 and men above 70 years old 2. Premature menopause (< 45 years of age) 3. Maternal family history of hip fracture 4. Low body mass index/BMI ( 5. Hyperthyroidism or hyperparathyroidism 6. Loss of height or hunched back 7. Prolonged immobilisation 8. Taking long-term steroidal medication |
| How to treat osteoporosis? |
| • Life style modification • Stop Smoking and Alcohol, exercise, intake of sufficient calcium and Vitamin D. • Drugs: There are many drugs which either improve bone formation or reduce bone resorption. Doctor will weigh the pros and cons and will prescribe the proper drug. Some of the examples of drugs are: Bisphosphonates (Alendronate,Resedronate), Raloxifene, Denosumab, Strontium ranelate.etc. |
Prepared by: IMU Clinical Campus students – Mohamed Hazimin Khalaff, Affendi Lee, Keerthena Kana Vathi, Ng Kha Sheng, Pavin A/L Rajanthran Advisor: Prof Esha Das Gupta