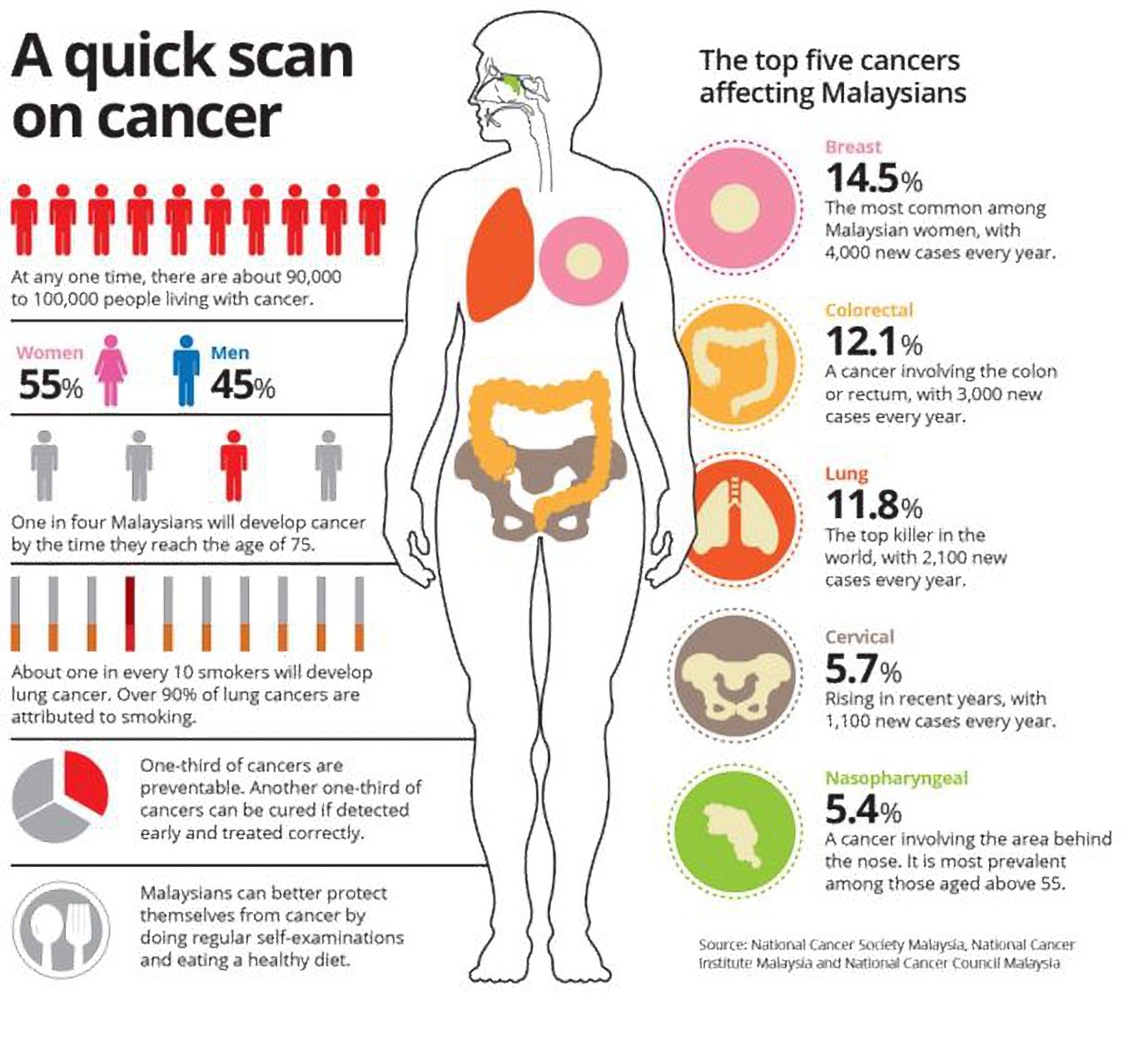
It is undeniable there is an increasing rate of Malaysians being diagnosed and battling the big C, with a majority of them being women. Based on the National Cancer Registry of Malaysia (NCR) records, 21,773 Malaysians are diagnosed with cancer. The Ministry of Health estimates that one in four Malaysians will develop cancer by the time they are 75 years old. Cancer is the bane of our existence, and while we can earnestly pray to be spared the agony, there are measures that can be taken for early detection.
Source: http://www.thestar.com.my/news/nation/2016/02/14/battling-the-big-c-health-ministry-making-plans/
Individuals with a high risk of cancer should talk to their family doctors and be educated and, empowered on how to reduce their risks from developing the cancer from young (primary prevention). A tumour marker test is never a screening test for cancer.
Adverse Effects of Tumour Marker as a Screening Test One may ask, “My tumour marker test result shows a low level, therefore, am I free of cancer?” Even high levels of tumour markers is not diagnostic of cancer, and it applies the same way with a low level reading as well. You cannot rely on it independently to determine that you are free from the disease, as these markers may potentially give false-positive or false-negative results. When you become too overwhelmed by the abnormal level of one tumour marker test, you may convince your doctor to focus solely on investigating if you are suffering from one type of cancer and miss out on other possibilities. Or even worse, despite getting a false-negative after a thorough process of many other invasive tests (with high costs), you may have trouble accepting that you’re truly cancer-free due to the emotional turmoil experienced from believing the tumour marker test. Thus, psychological complications or adverse effects such as generalised anxiety, excessive fear and major depressive disorders occur. Limitations of the Tumour Marker Test include:
- Many non-cancerous diseases can also elevate tumour marker levels.
- Some tumour marker levels have high baselines in normal individuals.
- It is difficult to obtain consistent results because tumour marker levels can change over time.
- The level of a tumour marker may not elevate until the cancer spreads (this is not helpful for early detection, screening, or observing for recurrence).
- Many common cancers do not produce tumour markers.
Questions to Ask the Doctor When you are deciding if a tumour marker test is necessary, here are a few suggested questions you may ask your doctor:
- Do you recommend that I undergo any tumour marker tests? If so, which ones?
- How are these tests performed? How often should I get tested?
- Can you explain the impact of the test results?
- If I have abnormal levels of a tumour marker, what does that mean? How does it affect my health?
- How will the tumour marker tests be used in my follow-up care?
- Where can I get more information about tumour markers?
Now that you are well-informed, you may save yourself from going through unnecessary anxiety by checking with your doctor if the tumour marker tests are necessary for you. Remember that these tests have their purposes and limitations, therefore, the results may sometimes fluctuate – indicating a false-positive or a false-negative. Should you have taken the test and if the levels are high, keep composed and speak to your doctor for an informed decision.
Reference: http://www.thestar.com.my/news/nation/2016/04/03/about-100000-malaysians-suffer-from-cancer-each-year/#0MCp4VbEhhacdbj7.99 http://www.cancer.net/navigating-cancer-care/diagnosing-cancer/tests-and-procedures/tumor-marker-tests http://www.breastcancer.org/symptoms/testing/types/blood_marker https://www.canc
er.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-fact-sheet http://www.moh.gov.my/images/gallery/Report/Cancer/MalaysiaCancerStatistics_2006.pdf Vetted and edited by Assoc Prof Dr Verna Lee Kar Mun Consultant Family Medicine Specialist, IMU This article is brought to you by IMU Healthcare.

