[fusion_builder_container hundred_percent=”no” equal_height_columns=”no” menu_anchor=”” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=”” background_color=”” background_image=”” background_position=”center center” background_repeat=”no-repeat” fade=”no” background_parallax=”none” parallax_speed=”0.3″ video_mp4=”” video_webm=”” video_ogv=”” video_url=”” video_aspect_ratio=”16:9″ video_loop=”yes” video_mute=”yes” overlay_color=”” overlay_opacity=”0.5″ video_preview_image=”” border_size=”” border_color=”” border_style=”solid” padding_top=”” padding_bottom=”” padding_left=”” padding_right=””][fusion_builder_row][fusion_builder_column type=”1_1″ layout=”1_1″ background_position=”left top” background_color=”” border_size=”” border_color=”” border_style=”solid” border_position=”all” spacing=”yes” background_image=”” background_repeat=”no-repeat” padding=”” margin_top=”0px” margin_bottom=”0px” class=”” id=”” animation_type=”” animation_speed=”0.3″ animation_direction=”left” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” center_content=”no” last=”no” min_height=”” hover_type=”none” link=””][fusion_text] As part of IMU’s Medical Programme’s Semester 5 curriculum, students are required to undertake a 4-week hospital placement. We were posted to several different hospitals in Malaysia. My group was posted to Hospital Sultanah Nora Ismail, Batu Pahat, in Johor. We rotated between different departments to gain an overview of how each department works, and the kinds of patients these departments manage. The departments included paediatrics, internal medicine, obstetrics and gynaecology, and surgery. To ensure our safety during the Covid-19 pandemic, our posting was cut short by 2 weeks. However, we still managed to learn a lot from this experience. [/fusion_text][fusion_imageframe image_id=”41965″ style_type=”none” stylecolor=”” hover_type=”none” bordersize=”15″ bordercolor=”#ffffff” borderradius=”” align=”none” lightbox=”no” gallery_id=”” lightbox_image=”” alt=”” link=”” linktarget=”_self” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=”” animation_type=”” animation_direction=”left” animation_speed=”0.3″ animation_offset=””]https://www.imu.edu.my/media/2020/10/Group-Pica.jpg[/fusion_imageframe][fusion_text] The posting included scheduled clinical case discussions and bedside teaching with the faculty professors at Hospital Sultanah Nora Ismail, Batu Pahat. Here, we presented patient cases and received feedback that helped us to modulate our thinking from that of preclinical students, to thinking more like clinical students or doctors working in the wards. The professors taught us to integrate the patient’s signs and symptoms with the theoretical knowledge that we had learnt in our pre-clinical semesters spent at Bukit Jalil. During bedside teaching, we were given the opportunity to demonstrate and refine our physical examination skills, and pick up positive signs which we may not have seen when practising on simulated patients, manikins or on fellow students. 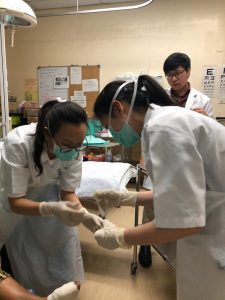 We also had procedure demonstrations where the nurse educator, Sister Nalini allowed us to assist and perform certain procedures such as venepuncture, nasogastric tube insertion and taking ECG and vital signs. This was a good experience for us to apply the skills we learnt and practiced in the Clinical Skills and Simulation Centre (CSSC) of the Bukit Jalil campus. In scheduled sessions with the staff of Hospital Sultanah Nora Ismail, Batu Pahat, we were also given the chance to apply our preclinical knowledge. We were required to be on-call from 5 through 10 pm in the Emergency Department at least once a week, to experience how healthcare professionals work together to diagnose and treat new patients. Here, we were able to assist the medical assistants in some procedures such as toilet and suturing (T&S), wound cleaning and urinary catheter insertion. I realized that the integrated preclinical curriculum in IMU had prepared us well for basic procedures and this gave me the confidence to step up to the task when I had a chance to apply my knowledge and skills. Interacting with real patients in the hospital setting is very different from interacting with simulated patients in the CSSC. However, the knowledge that we have gained remains applicable. This hospital posting allowed us to reinforce our history-taking skills, and to apply physical examination skills to obtain a diagnosis. Since Day 1 of enrolling into IMU, the clinical skills faculty have always emphasized on the importance of effective communication with patients, to ensure that patients are comfortable and willing to share their story. I found that most of us, IMU medical students, were coherent and confident in history taking, apart from challenges of the language barrier. In the CSSC, we typically speak to simulated patients who present with classic symptoms of a specific condition. However, at Hospital Sultanah Nora Ismail, Batu Pahat, we were confronted with various presentations of the same diseases, teaching us to broaden our mindsets. Learning the classical presentation is still an important first step as it helps guide our history taking, so we know to rule out certain conditions and to bring ourselves to a conclusion regarding the patient’s illness.
We also had procedure demonstrations where the nurse educator, Sister Nalini allowed us to assist and perform certain procedures such as venepuncture, nasogastric tube insertion and taking ECG and vital signs. This was a good experience for us to apply the skills we learnt and practiced in the Clinical Skills and Simulation Centre (CSSC) of the Bukit Jalil campus. In scheduled sessions with the staff of Hospital Sultanah Nora Ismail, Batu Pahat, we were also given the chance to apply our preclinical knowledge. We were required to be on-call from 5 through 10 pm in the Emergency Department at least once a week, to experience how healthcare professionals work together to diagnose and treat new patients. Here, we were able to assist the medical assistants in some procedures such as toilet and suturing (T&S), wound cleaning and urinary catheter insertion. I realized that the integrated preclinical curriculum in IMU had prepared us well for basic procedures and this gave me the confidence to step up to the task when I had a chance to apply my knowledge and skills. Interacting with real patients in the hospital setting is very different from interacting with simulated patients in the CSSC. However, the knowledge that we have gained remains applicable. This hospital posting allowed us to reinforce our history-taking skills, and to apply physical examination skills to obtain a diagnosis. Since Day 1 of enrolling into IMU, the clinical skills faculty have always emphasized on the importance of effective communication with patients, to ensure that patients are comfortable and willing to share their story. I found that most of us, IMU medical students, were coherent and confident in history taking, apart from challenges of the language barrier. In the CSSC, we typically speak to simulated patients who present with classic symptoms of a specific condition. However, at Hospital Sultanah Nora Ismail, Batu Pahat, we were confronted with various presentations of the same diseases, teaching us to broaden our mindsets. Learning the classical presentation is still an important first step as it helps guide our history taking, so we know to rule out certain conditions and to bring ourselves to a conclusion regarding the patient’s illness.
Overall, I really enjoyed being in the hospital. It is truly a place where one can find fulfilment in interacting with patients and helping them get well. It was one of the postings that I was looking forward to, and this experience has given me the confidence to look forward to the clinical phase of my studies using the skills that I have acquired over the past 5 semesters.
Written by Carmen Ching
This article is submitted by the Clinical and Experiential Learning Sub-committee.
[/fusion_text][/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]

