Third year IMU medical student, Andy Chuang, had the opportunity to undergo a 4-week medical elective at Kaohsiung Medical University Chung-Ho Memorial Hospital, Taiwan. Here, he relates to us his experience in Taiwan. Healthcare in Taiwan is different as compared to Malaysia or the UK. General Practice (GP) sector is nowhere to be seen in Taiwan therefore due to the lack of filter, anyone with any medical condition can present themselves and demand for medical treatment at the hospital. Most of these cases were referred to the Outpatient Clinic located at the Accident & Emergency Department. In addition, Taiwan has its own integrated National Health Insurance (NHI). It was founded based on the concept of mutual assistance and depends on the insured paying their premiums according to regulations. By law, every Taiwanese citizen with official residency or foreign nationals living in Taiwan with a resident certificate, regardless of age, gender, or employment status, must enroll into the programme. When people fall ill, the government uses the premiums it receives to help patients pay part of their medical and medication costs to the contracted healthcare institutions. Although born a Taiwanese, I never had the chance to expose myself to the healthcare system in Taiwan. While waiting for my transfer to University of Dundee UK, I had the privilege to spend a total of four weeks at the Department of Gastroenterology and Department of Hepatobiliary, Chung-Ho Memorial Hospital under the Faculty of Medicine, Kaohsiung Medical University. The Chung-Ho Memorial Hospital is currently the largest medical center and considered as the most prestigious institution of medical education in the Southern region of Taiwan.
It was a great honor for me to learn at their institution and gain new experiences that I have never encountered before.
Work started at 7:30am every day, where I would join the clerk, intern and resident doctors for a meeting. Each morning one or two patient’s case would be discussed by the patient’s doctor in charge. To make the session more exciting, the presenting doctor would sometimes throw questions to the audiences (targeting the young doctors and clerk mainly). This is where I obtained a lot of clinical knowledge and take home messages. Besides ward work and following my mentor, I was able to join lectures and tutorials with medical students from the Faculty of Medicine, Kaohsiung Medical University. 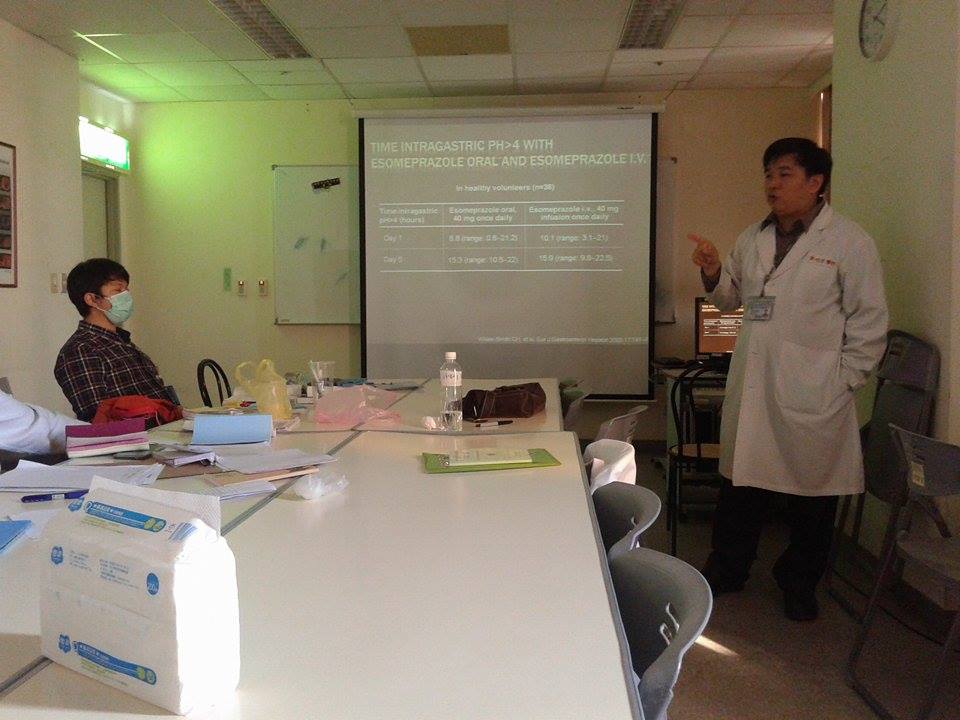

 All consultations with patients and ward round discussions were conducted in Chinese and Hokkien, which I took some time to adapt myself to an ‘all Chinese’ healthcare environment. Patients’ records were all in English and stored in a computer system which can be easily accessed by doctors using any computers within the hospital. This was extremely convenient, as a patient can be sent from one department to another, doctor from another department can immediately look into the case. Another good thing about this system was that, clerks like us were able to access the database as well hence it facilitated our learning. We can also refer to reports recorded by doctors.
All consultations with patients and ward round discussions were conducted in Chinese and Hokkien, which I took some time to adapt myself to an ‘all Chinese’ healthcare environment. Patients’ records were all in English and stored in a computer system which can be easily accessed by doctors using any computers within the hospital. This was extremely convenient, as a patient can be sent from one department to another, doctor from another department can immediately look into the case. Another good thing about this system was that, clerks like us were able to access the database as well hence it facilitated our learning. We can also refer to reports recorded by doctors.  During my two weeks attachment at the Department of Gastroenterology, I had the opportunity to expose myself to many gastrointestinal diseases including diseases I’ve never seen before during my past attachments. Given a role as a clerk, I was assigned to a patient whom I had to keep track of his/her progress until discharge. In addition, I was fortunate to see many esophagogastroduodenoscopy (EGD) procedures and even performing it onto a dummy model during teaching sessions. Together with EGD, I have also observed procedures like esophageal variceal banding, argon plasma coagulation and local injection of hyaline saline-epinephrine.
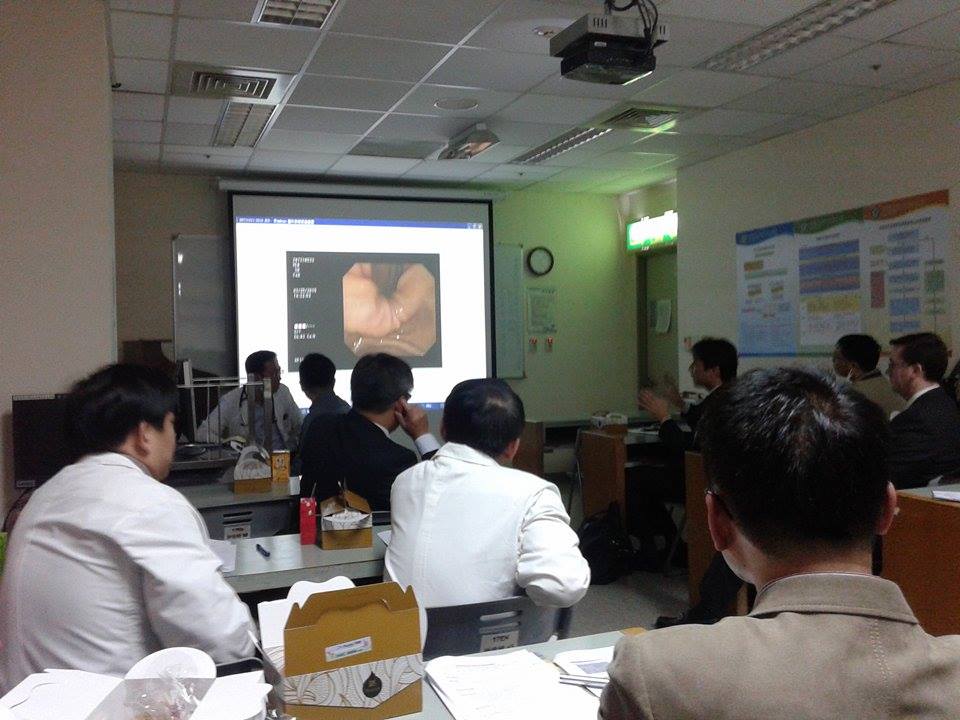
During my two weeks attachment at the Department of Gastroenterology, I had the opportunity to expose myself to many gastrointestinal diseases including diseases I’ve never seen before during my past attachments. Given a role as a clerk, I was assigned to a patient whom I had to keep track of his/her progress until discharge. In addition, I was fortunate to see many esophagogastroduodenoscopy (EGD) procedures and even performing it onto a dummy model during teaching sessions. Together with EGD, I have also observed procedures like esophageal variceal banding, argon plasma coagulation and local injection of hyaline saline-epinephrine. ![IMG_20160201_114448[1]](https://www.imu.edu.my/media/2016/02/IMG_20160201_1144481.jpg) Dr Wu was my mentor at the Department of Gastroenterology. During the two weeks attachment in this department, Dr Wu took a keen interest in my progress. Having an unsatisfactory amount of clinical knowledge in me, she was still very patient and would explain each patient’s case before the patient walks in and treatment option when the patient walks out. She understood the difficulties I was facing; having studied in an environment that had a different language. Showing genuine care for her patients and being enthusiastic to colleagues, Dr Wu had earned much respect and took pride in her chosen profession. It was also Dr Wu that gave me the opportunity to join the weekly departmental meetings and the monthly Southern District Gastroenterology and Hepatobiliary Preservation Society Meeting that was attended by consultants, surgeons and professors from foreign countries like Japan and USA. Difficult cases were discussed in the meeting, giving me the chance to witness how the closest possible diagnosis and differentials were made through logical clinical reasoning.
Dr Wu was my mentor at the Department of Gastroenterology. During the two weeks attachment in this department, Dr Wu took a keen interest in my progress. Having an unsatisfactory amount of clinical knowledge in me, she was still very patient and would explain each patient’s case before the patient walks in and treatment option when the patient walks out. She understood the difficulties I was facing; having studied in an environment that had a different language. Showing genuine care for her patients and being enthusiastic to colleagues, Dr Wu had earned much respect and took pride in her chosen profession. It was also Dr Wu that gave me the opportunity to join the weekly departmental meetings and the monthly Southern District Gastroenterology and Hepatobiliary Preservation Society Meeting that was attended by consultants, surgeons and professors from foreign countries like Japan and USA. Difficult cases were discussed in the meeting, giving me the chance to witness how the closest possible diagnosis and differentials were made through logical clinical reasoning.  Dr Yeh was my mentor at the Department of Hepatobiliary in the remaining two weeks. On the first meet up, Dr. Yeh helped me familiarise myself with the most encountered diseases in the Hepatobiliary department, in particular revising the knowledge I have on viral hepatitis infection, cirrhosis and hepatocellular carcinoma (HCC) that is all of high prevalence in Taiwan. I felt really comfortable learning beside Dr Yeh because of his easy-going personality and was incredibly approachable and keen to teach.
Dr Yeh was my mentor at the Department of Hepatobiliary in the remaining two weeks. On the first meet up, Dr. Yeh helped me familiarise myself with the most encountered diseases in the Hepatobiliary department, in particular revising the knowledge I have on viral hepatitis infection, cirrhosis and hepatocellular carcinoma (HCC) that is all of high prevalence in Taiwan. I felt really comfortable learning beside Dr Yeh because of his easy-going personality and was incredibly approachable and keen to teach.  I was given the chance to see many ultrasonography procedures when I was with Dr Yeh. With no prior education in ultrasonography, I found it difficult to interpret the images. Fortunately, with proper guidance from Dr Yeh and self-directed learning, I have learnt the basics of interpretation of abdominal ultrasonography images within 2 weeks. With the need of ultrasonography for guidance, I have assisted in simple procedures like paracentesis and observe treatment
I was given the chance to see many ultrasonography procedures when I was with Dr Yeh. With no prior education in ultrasonography, I found it difficult to interpret the images. Fortunately, with proper guidance from Dr Yeh and self-directed learning, I have learnt the basics of interpretation of abdominal ultrasonography images within 2 weeks. With the need of ultrasonography for guidance, I have assisted in simple procedures like paracentesis and observe treatment
procedures like percutaneous ethanol injection therapy and radiofrequency tumor ablation. I have gained so much invaluable experiences through the exploration of the principles of healthcare beyond those in Malaysia. I have to admit that it was not easy for a young Year 3 student to attempt a clinical elective. It was the eagerness to learn that had kept me going through the four weeks. Many unfamiliar things were jotted down right on the spot and studied immediately through the internet and Pocket Medicine in the evening after working hours, in order to keep up with case discussions and not let my mentor down. All I wanted was to get better and better each day.
In conclusion, I would like to thank IMU who gave me a stable foundation in pre-clinical knowledge as well as everyone who I had the good fortune to briefly cross paths with during this elective programme.


No approved comments.