For World Diabetes Day 2016, the International Diabetes Federation (IDF) has launched the campaign under the theme Eyes on Diabetes, focusing on two key messages: Screening for type 2 diabetes is important to modify its course and reduce the risk of complications; and Screening for diabetes complications is an essential part of managing type 1 and type 2 diabetes
IDF has estimated that globally as many as 193 million people, or close to half of all adults living with diabetes in 2015, are unaware of their disease. Most of these cases are type 2 diabetes.
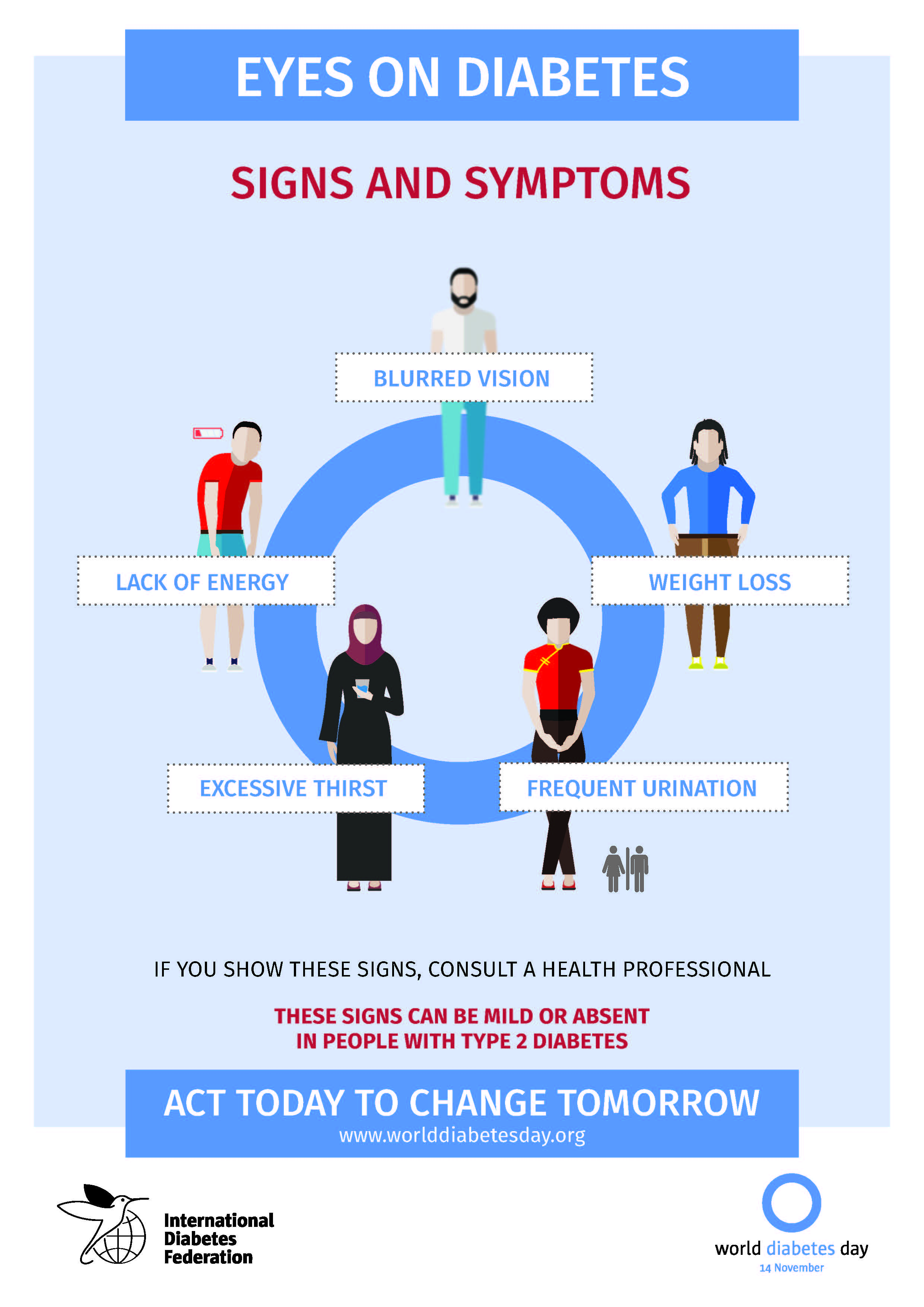
Malaysian statistics are equally grim. The National Health and Morbidity Survey (NHMS) estimated that 17.5%* of Malaysians between the ages of 20 to 79 suffered from diabetes. The Ministry of Health’s Diabetes database of people newly diagnosed with diabetes says 2.1% come from the 18-29-year-old age group, while 20.1% are aged 30-44 years. The largest segment, 35%, are from the newly diagnosed diabetics of 45-54-year-old age group, while people aged 55-64 are the second highest group at 28.7%. The final group culminating in those 65-79 years old comes in at 15.2%. All age segments show a huge increase, underscoring the futility of all public service announcements and health outreach initiatives embarked on by both public and private healthcare organisations and companies. On top of that, there already are an estimated 3.3 million diabetics in the country while there are also roughly 1.7 million people living with undiagnosed diabetes. A person with type 2 diabetes can live for several years without showing any symptoms, during which time high blood glucose is silently damaging the body. There is, therefore, an urgent need to screen, diagnose and provide appropriate treatment to people with diabetes. Thus, the earlier a person is diagnosed, the earlier treatment can be initiated in order to reduce the risk of harmful and costly complications. 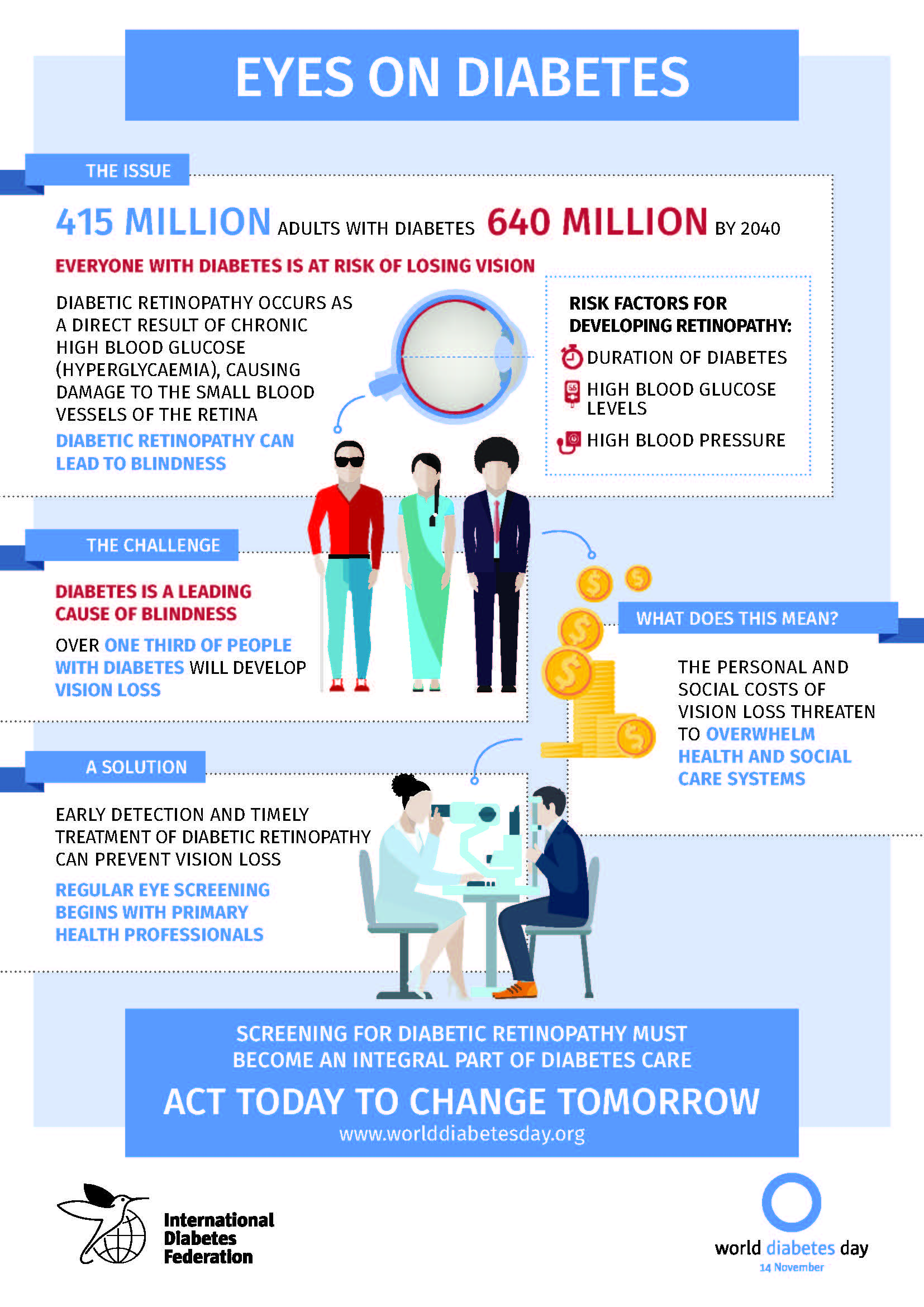 So why aren’t Malaysians taking their health and blood sugar more seriously? Endocrinologist, Dr Loh Vooi Lee of IMU Healthcare, puts it down to general apathy. “We make eating part of our culture more than we have made testing for diabetes a norm. Diabetes education, also known as diabetes self-management education and support (DSME/S), is defined as a collaborative process through which people with or at risk for diabetes gain the knowledge and skills needed to modify behaviour and successfully self-manage the health issues and its related conditions. In Malaysia, all healthcare providers have an educational role when caring for people with diabetes,” he says.
So why aren’t Malaysians taking their health and blood sugar more seriously? Endocrinologist, Dr Loh Vooi Lee of IMU Healthcare, puts it down to general apathy. “We make eating part of our culture more than we have made testing for diabetes a norm. Diabetes education, also known as diabetes self-management education and support (DSME/S), is defined as a collaborative process through which people with or at risk for diabetes gain the knowledge and skills needed to modify behaviour and successfully self-manage the health issues and its related conditions. In Malaysia, all healthcare providers have an educational role when caring for people with diabetes,” he says.
He also thinks that people avoid testing for diabetes because they are worried about the problems associated with the disease.
Dr Loh stresses that it is better to find out sooner and be treated as quickly as possible because it is better for an individual in the long run. “Ninety percent of the time type 2 diabetes is picked up during a screening when a person has had no symptoms at all. Malaysians only seek medical help when something happens. Otherwise, they do not volunteer themselves for blood tests.” “However, we are such a high risk population that testing should be something anyone above the age of 30 should be required to undergo. Diabetes can bring about complications that affect the big blood vessels of the body such as the heart and the brain. It also affects the small blood vessels in the kidneys, eyes and nerves. Early diagnosis of diabetes means we can quickly treat the condition and prevent the complications. The cost of treating a person as an in-patient is ten times more than if they are treated as an out-patient. Being treated only when complications manifest does not benefit either the patient or the country because of the cost,” asserts Dr Loh. 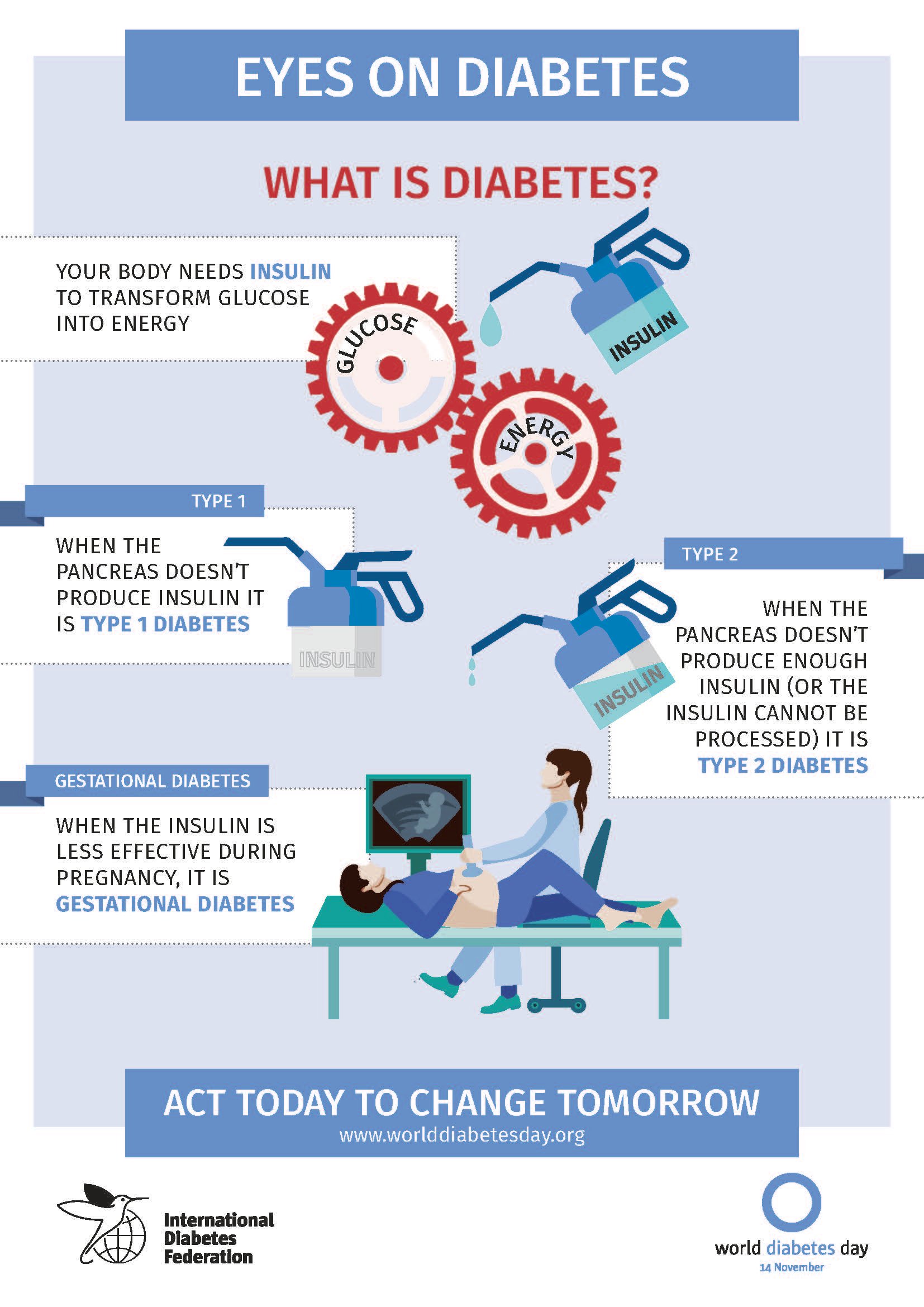 Simple but under-utilised screening Screening for diabetes is simple and fast. All it requires is to fast for a period of eight to nine hours before a blood test, or, if you have eaten, to be tested for random blood sugar or HbA1c. The term HbA1c refers to glycated haemoglobin. It develops when haemoglobin, a protein within red blood cells that carries oxygen throughout your body, joins with glucose in the blood, becoming ‘glycated’. By measuring glycated haemoglobin (HbA1c), doctors are able to get an overall picture of what a person’s average blood sugar levels have been over a period of weeks/months. It is an easily requested test that can be done at any pathology lab, and yet, not enough people are getting tested. This general apathy is a big part of the reason that diabetes-related diseases and complications are draining public healthcare resources, and resulting in major health complications and morbidity.
Simple but under-utilised screening Screening for diabetes is simple and fast. All it requires is to fast for a period of eight to nine hours before a blood test, or, if you have eaten, to be tested for random blood sugar or HbA1c. The term HbA1c refers to glycated haemoglobin. It develops when haemoglobin, a protein within red blood cells that carries oxygen throughout your body, joins with glucose in the blood, becoming ‘glycated’. By measuring glycated haemoglobin (HbA1c), doctors are able to get an overall picture of what a person’s average blood sugar levels have been over a period of weeks/months. It is an easily requested test that can be done at any pathology lab, and yet, not enough people are getting tested. This general apathy is a big part of the reason that diabetes-related diseases and complications are draining public healthcare resources, and resulting in major health complications and morbidity.
“The first five to ten years of uncontrolled diabetes can result in coronary failure or stroke. Diabetes is generally a long-standing disease, but when it is finally diagnosed, 10 to 20 percent of people would already have complications,” states Dr Loh.
 Effective management of diabetes is the key to ensuring patients do not become a health statistic. People with diabetes and their families and caregivers have a great deal to learn in order to become effective self-managers of their diabetes. Endocrinologists, Family Medicine practitioners and General Practitioners can help by explaining the diabetes disease process and treatment options and helping patients incorporate nutritional management and physical activity into the patient’s lifestyle. A doctor should also advise patients on using medication safely and for maximum therapeutic effectiveness, explaining dosage and consumption times clearly. Doctors can also help a patient set health goals which can be measured against their blood sugar readings, weight and exercise accomplishments.
Effective management of diabetes is the key to ensuring patients do not become a health statistic. People with diabetes and their families and caregivers have a great deal to learn in order to become effective self-managers of their diabetes. Endocrinologists, Family Medicine practitioners and General Practitioners can help by explaining the diabetes disease process and treatment options and helping patients incorporate nutritional management and physical activity into the patient’s lifestyle. A doctor should also advise patients on using medication safely and for maximum therapeutic effectiveness, explaining dosage and consumption times clearly. Doctors can also help a patient set health goals which can be measured against their blood sugar readings, weight and exercise accomplishments.
However, the onus is on the patient to commit to any plan which will help them manage their disease effectively. This is particularly true in the change of diet needed, and the lifestyle modification (eating at regular times, controlling carbohydrate and sugar intake, increasing or starting regular exercise) needed to effectively curb diabetes.
“Diabetes education is so important, but it is not driven home hard enough in Malaysia. Malaysians need a medical catastrophe in life before they take action,” says Dr Loh grimly. “Contrary to any claims a person may see on social media, there is no cure for diabetes,” he stresses. He emphasises the need for screening because not only will it identify diabetes, but also because screenings can help pick up other issues, resulting in cost savings when treatment is done at an early stage. “If diabetes is treated aggressively in the first five years, a patient can benefit from it up to 15 years into living with the condition. This al
so makes treatment more cost effective. When diabetes is picked up at an early stage, doctors can help slow or reverse its effects. We should not just be treating heart attacks which are a result of diabetes; we should be aggressively tackling it in its early stages,” Dr Loh says. 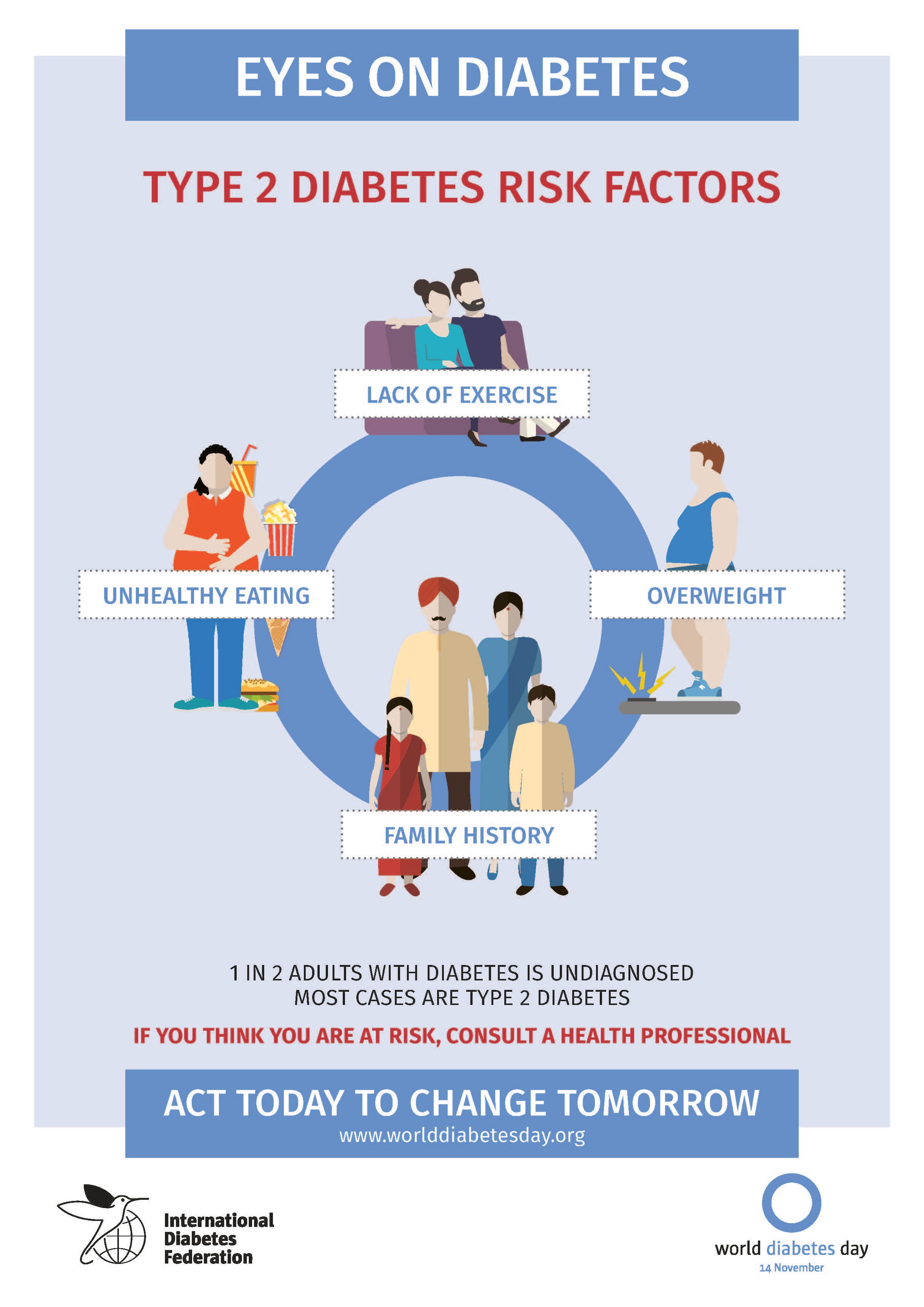 He goes on to relate how he was able to work with one of his patients who had very poor diabetes control. “This 35-year-old, heavy Chinese male was diabetic for half a year, with very poor control, even though he was on injected insulin. He was admitted to hospital in a diabetic coma. He decided to take a very aggressive, proactive approach in his treatment and together we planned lifestyle changes which included diet and exercise. He was able to lose weight and to come off insulin and his disease is now very well-controlled,” Dr Loh shares. He stresses that while it is rare for a person with diabetes to fully come off medication, there is a possibility of reducing dosage, or even getting a person off injectable insulin and onto oral medication if detection and lifestyle modifications are done in earnest.
He goes on to relate how he was able to work with one of his patients who had very poor diabetes control. “This 35-year-old, heavy Chinese male was diabetic for half a year, with very poor control, even though he was on injected insulin. He was admitted to hospital in a diabetic coma. He decided to take a very aggressive, proactive approach in his treatment and together we planned lifestyle changes which included diet and exercise. He was able to lose weight and to come off insulin and his disease is now very well-controlled,” Dr Loh shares. He stresses that while it is rare for a person with diabetes to fully come off medication, there is a possibility of reducing dosage, or even getting a person off injectable insulin and onto oral medication if detection and lifestyle modifications are done in earnest.
“Diabetes does not discriminate. It is a killer disease. It is also a socially and economically affecting disease, with the cost of medication going up year by year.”
“With medication starting at RM200 per month and other add-on medicines costing another RM200, the cost of the treatment for diabetes is easily ten times more than it was ten years ago. We need to encourage enough lifestyle changes, and emphasise the importance of early screening so that Malaysians can enjoy a better quality of life. Early detection would enable us to better educate the patient, which is a pre-cursor to effective diabetes management,” concludes Dr Loh. * Note: Statistics are based on the latest updates from NHMS 2015 This article is brought to you by IMU Healthcare.


No approved comments.